Manual Muscle Testing Shoulder
Manual muscle testing is used in rehabilitation and recovery to evaluate contractile units, including muscles and tendons, and their ability to generate forces. When used as part of rehabilitation, muscle testing is an important evaluative tool to assess impairments and deficits in muscle performance, including strength, power, or endurance. Depress the shoulder girdle by attachment on humerus, & obliquely aduct the humerus toward the opposite iliac crest Action of Muscle as a Whole With the origin fixed, it. “Move your arm out to the side.” Here, in testing shoulder abduction, the patient will be positioned in supine to perform the test in the horizontal plane. The tester will support the arm to minimize the friction between the arm and the testing surface, and provide stabilization at the upper trapezius if needed.
Manual Muscle Testing Grading System. Grading Scale Range: 0 to 5: 0: None: No visible or palpable contraction: 1: Trace: Visible or palpable contraction with.
Abstract
Mmt For Shoulder
Introduction
A body of basic science and clinical research has been generated on the manual muscle test (MMT) since its first peer-reviewed publication in 1915. The aim of this report is to provide an historical overview, literature review, description, synthesis and critique of the reliability and validity of MMT in the evaluation of the musculoskeletal and nervous systems.
Methods
Online resources were searched including Pubmed and CINAHL (each from inception to June 2006). The search terms manual muscle testing or manual muscle test were used. Relevant peer-reviewed studies, commentaries, and reviews were selected. The two reviewers assessed data quality independently, with selection standards based on predefined methodologic criteria. Studies of MMT were categorized by research content type: inter- and intra-examiner reliability studies, and construct, content, concurrent and predictive validity studies. Each study was reviewed in terms of its quality and contribution to knowledge regarding MMT, and its findings presented.
Results
More than 100 studies related to MMT and the applied kinesiology chiropractic technique (AK) that employs MMT in its methodology were reviewed, including studies on the clinical efficacy of MMT in the diagnosis of patients with symptomatology. With regard to analysis there is evidence for good reliability and validity in the use of MMT for patients with neuromusculoskeletal dysfunction. The observational cohort studies demonstrated good external and internal validity, and the 12 randomized controlled trials (RCTs) that were reviewed show that MMT findings were not dependent upon examiner bias.
Conclusion
The MMT employed by chiropractors, physical therapists, and neurologists was shown to be a clinically useful tool, but its ultimate scientific validation and application requires testing that employs sophisticated research models in the areas of neurophysiology, biomechanics, RCTs, and statistical analysis.
Review
The role of the muscle system in spinal function has become increasingly well acknowledged. Manual muscle testing (MMT) as a method of diagnosis for spinal dysfunction has not been well utilized. This paper will present evidence that the MMT can be a legitimate and useful evaluation tool for the assessment of the musculoskeletal and nervous systems.
There are many ways of examining the nervous system and the musculoskeletal system. It has been proposed that the term neuromusculoskeletal system be adopted because examination of the one may reflect the status of the other [1,2]. The evaluation methods of many manipulative therapists often focus at either end of the nervous system, and this paper suggests that MMT provides a method of examining both (the central and the peripheral) ends.
MMT is the most commonly used method for documenting impairments in muscle strength. Limited muscle testing methods are taught in a number of chiropractic schools around the world, however in 2006 a major 'stand alone' chiropractic technique that employs MMT for the evaluation of patients known as applied kinesiology chiropractic technique (AK), turned 42 years old. We propose in this review to look at the research status of MMT in the manual examination of the nervous system's status. The early years of the AK method are related elsewhere in detail []. The specific protocols and clinical objectives of the technique have been described in previous publications [-9].
AK has therefore been used by a proportion of the chiropractic profession for over 42 years and is now used by other healing professions. In a survey by the National Board of Chiropractic Examiners in 2000, 43.2% of respondents stated that they used applied kinesiology in their practices, up from 37.2% of respondents who reported they used AK in 1991, [10-12] with similar numbers reported in Australia [13]. The general public's awareness of MMT and AK has also been increased worldwide by virtue of the patient education program Touch for Health (T4H) designed by an International College of Applied Kinesiology (ICAK) diplomate, John Thie. T4H was one of the first public self-help programs and there are claims that it is the fastest growing 'body work' program in the world, used by over 10 million people [14].
For the purposes of this review we define MMT as a diagnostic tool and AK as a system for its use and therapy based on the findings of the MMT
In this paper we pose the following questions: 1) 'Is the MMT approach worthy of scientific merit?' and 2) 'How can new diagnostic and treatment techniques employing MMT be critiqued for scientific merit?' and 3) 'Does this evidence add scientific support to chiropractic techniques (such as AK) that employ the MMT?'
Another main objective of this literature review was to investigate the evidence for intraexaminer reliability, interexaminer reliability, and validity of MMT in the assessment of patients.
Methods
Online resources were searched using Pubmed and CINAHL (Cumulative Index to Nursing and Allied Health literature). The search terms 'manual muscle test', 'manual muscle testing', and 'applied kinesiology' found over 100 articles in which the MMT was used to document strength in patients with 17 (primarily pain related) diseases/disorders, ranging from low back pain and sacroiliac joint pain to neck pain, post-whiplash syndrome, knee, foot, and shoulder pain, and included MMT for the evaluation of patients with post-polio syndrome, amyotrophic lateral sclerosis, muscular dystrophy, cerebral palsy, Down syndrome, mastalgia, hypothyroidism, dysinsulinism, enuresis and several other disorders of childhood.
After abstracts were selected for relevance and the papers acquired and reviewed, the literature was sorted according to relevance and quality. Inclusion criteria were that the report had a Cohen's kappa coefficient of 0.50 or higher (the magnitude of the effect size shown in the study to be significant) in regards to the intra- and inter-examiner reliability, and/or the validity (construct and content validity, convergent and discriminant validity, concurrent and predictive validity). This selection criteria is consistent with the one suggested by Swinkels et al for the evaluation of the quality of research literature []. Randomized clinical trials (n = 12), prospective cohort studies (n = 26), retrospective studies (n = 17), cross-sectional studies (n = 26), case control studies (n = 10), and single-subject case series and case reports (n = 19) were the types of studies reviewed. Studies with a control group (a randomized clinical trial), examiner blinding, and pre- and post-test design are indicated in the descriptions of each study. Duplicates and articles published in non-peer-reviewed literature were excluded.
Statistical presentations of the data are presented showing the average correlation coefficients of MMT examination upon the different patient populations for each study.
Operational Definitions and History of the Manual Muscle Test
In order to be meaningful, all measurements must be based on some type of operational definition. An operational definition is a description of the methods, tools, and procedures required to make an observation (i.e. a definition that is specific and allows objective measurement). Kaminsky and Fletcher et al provide clinicians with some strategies to critically analyze the scientific merit of manual therapies [,17].
A basic understanding of operational definitions is required in order to make judgments about the methods used in articles and to know which research findings should be implemented in practice. For example, how should we judge the value of the MMT for the gluteus maximus or gluteus medius muscles in cases of sacroiliac joint pain and dysfunction, knowing that statements range from 'weakness of the gluteals is usually present in dysfunction of the sacroiliac joint' (Janda 1964) [18] to 'the results of this study cast doubt on the suitability of manual muscle testing as a screening test for strength impairments'? (Bohannon 2005) [].
Within the chiropractic profession, the ICAK has established an operational definition for the use of the MMT:
'Manual muscle tests evaluate the ability of the nervous system to adapt the muscle to meet the changing pressure of the examiner's test. This requires that the examiner be trained in the anatomy, physiology, and neurology of muscle function. The action of the muscle being tested, as well as the role of synergistic muscles, must be understood. Manual muscle testing is both a science and an art. To achieve accurate results, muscle tests must be performed according to a precise testing protocol. The following factors must be carefully considered when testing muscles in clinical and research settings:
• Proper positioning so the test muscle is the prime mover
• Adequate stabilization of regional anatomy
• Observation of the manner in which the patient or subject assumes and maintains the test position
• Observation of the manner in which the patient or subject performs the test
• Consistent timing, pressure, and position
• Avoidance of preconceived impressions regarding the test outcome
• Nonpainful contacts – nonpainful execution of the test
• Contraindications due to age, debilitative disease, acute pain, and local pathology or inflammation'
In physical therapy research, the 'break test' is the procedure most commonly used for MMT, and it has been extensively studied [20-22]. This method of MMT is also the main test used in chiropractic, developed originally from the work of Kendall and Kendall [21,23].
In physical therapy the 'break test' has the following operational definition [20-22]. The subject is instructed to contract the tested muscle maximally in the vector that 'isolates' the muscle. The examiner resists this pressure until the examiner detects no increase in force against his hand. At this point an additional small force is exerted at a tangent to the arc created by the body part being tested. The initial increase of force up to a maximum voluntary strength does not exceed 1 sec., and the increase of pressure applied by the examiner does not exceed a 1-second duration. 'Strong' muscles are defined as those that are able to adapt to the additional force and maintain their contraction with no weakening effect. 'Weak' muscles are defined as those unable to adapt to the slight increase in pressure, i.e., the muscle suddenly becomes unable to resist the test pressure.
For example in the seated test for the rectus femoris muscle, a seated subject is asked to flex his knee toward his chest 10 degrees; when that position is reached, the examiner applies resistance at the knee, trying to force the hip to 'break' its hold and move the knee downward into extension. The ability of a muscle to lengthen but to generate enough force to overcome resistance is what is qualified by the examiner and termed 'Strong' or 'Weak.'
The grading system is based on muscle performance in relation to the magnitude of manual resistance applied by the examiner. Scores are ranked from no contraction to a contraction that can be performed against gravity and can accept 'maximal' resistance by the examiner, depending on the size of the muscle and the examiner's strength. However, in the AK use of MMT the implication of grades is limited to an interpretation of 'better' or 'worse', 'stronger' or 'weaker,' and no assumption is made about the magnitude of difference between grades.
MMT procedures are also commonly employed in clinical neurology as a means of subjectively evaluating muscle function. The examiner in the application of force to the subject's resistance evaluates the muscle groups being studied as subjectively 'weak' or 'strong' on a 5-point scale [24].
MMT is employed by physical therapists to determine the grades of strength in patients with pathological problems and neurologic or physical injuries (strokes, post-polio syndromes, fractures, post-surgical disabilities, etc.). The physical therapist's patients are often initially examined by a medical doctor who supervises the physical therapist's rehabilitation programs that may involve isometric, isokinetic, and isotonic muscle training regimes for the gradual rehabilitation of muscle function (often involving instruments and machinery).
In the absence of a pathological neurological deficit (pathological deficits were originally what physicians sought to find using MMT), [25,26] clinical inferences are made based upon the result of the MMT. This method of MMT is used in both chiropractic and physical therapy to determine a patient's progress during therapy [-9,20-23].
MMT, when employed by AK chiropractors, is used to determine whether manipulable impairments to neurological function (controlling muscle function) exist. For example, chiropractic management using MMT for a patient with carpal tunnel syndrome could involve assessment of the opponens policis and flexor digiti minimi muscles (innervated by the median and radial nerves), and then adjustment as indicated to the carpal bones, the radius and ulna, attention to an inhibited (on MMT) pronator teres muscle, adjustment of the cervical or thoracic spines, and evaluation of cranial nerve XI through MMT of the sternocleidomastoid and upper trapezius muscles. Any or all of these factors may require treatment in order to strengthen the inhibited opponens policis and flexor digiti minimi muscles that are evidence of the carpal tunnel syndrome. This 'continuous nervous system' thinking and testing may allow the identification of contributing sites to a pain state.
The expectation in a chiropractic setting is that the proper therapy will immediately improve muscle strength upon MMT, taking the patient from 'weak' to 'strong.' This is the reason that in most chiropractic settings, the grading system of muscle evaluation does not have as much significance as it does in physical therapy settings. Chiropractic therapy may produce rapid responses for the innervation of muscles because the basic therapy required for chiropractic patients is decompression of the nervous system. It is purported that this can be done readily with chiropractic manipulative therapy (CMT) [-].
When performed by an examiner's hands MMT may not be just testing for actual muscle strength; rather it may also test for the nervous system's ability to adapt the muscle to the changing pressure of the examiner's test. A nervous system functioning optimally will immediately attempt to adapt a muscle's activity to meet the demands of the test. There appears to be a delay in the recruitment of muscle motor units when the nervous system is functioning inadequately [,-,]. This delay varies with the severity of the nervous system's impairment, and influences the amount of weakness shown during the MMT.
Determining the ideal operational definition of a MMT can be difficult given the large number of test variations that exist. All of the tests described by Kendall, Wadsworth, Goodheart, Walther and others [,20-23] involve multiple joint movements and handling techniques. This results in a large number of variables that are difficult to control.
Because of the variability possible during a MMT, several studies examining MMT have used specialized instrumentation to provide support for the extremity tested and for standardization of joint position. Throughout its history manual muscle testing has been performed by practitioners' hands, isokinetic machines, and other handheld devices. However, isokinetic machines and dynamometers for more objective testing of muscles are still too expensive or cumbersome for clinical use, but this equipment is useful for research purposes [20-23].
Kendall et al (1993) [21] state:
'As tools, our hands are the most sensitive, fine tuned instruments available. One hand of the examiner positions and stabilizes the part adjacent to the tested part. The other hand determines the pain-free range of motion and guides the tested part into precise test position, giving the appropriate amount of pressure to determine the strength. All the while this instrument we call the hand is hooked up to the most marvelous computer ever created. It is the examiner's very own personal computer and it can store valuable and useful information of the basis of which judgments about evaluation and treatment can be made. Such information contains objective data that is obtained without sacrificing the art and science of manual muscle testing to the demand for objectivity.'
According to Walther (1988) [23]:
'Presently the best 'instrument' to perform manual muscle testing is a well-trained examiner, using his perception of time and force with knowledge of anatomy and physiology of muscle testing.'
Regardless of the methods or equipment one uses to standardize MMT in a clinical or research setting, it is most important that the test protocol be highly reproducible by the original examiner and by others.
Results
Research on the Reliability of the MMT
One way researchers determine if a clinical test is consistent and repeatable over several trials is to analyze its reliability. The reliability of a diagnostic method is the consistency of that measurement when repeated. Depending on the type of measurement that is performed, different types of reliability coefficients can be calculated. In all coefficients, the closer the value is to 1, the higher the reliability. For instance, calculating Cohen's kappa coefficient allows the researcher to determine how much agreement existed between two or more doctors performing MMT on patients with low back pain. A value greater than .75 indicates 'excellent' agreement, a value between .40 and .75 indicates 'fair to good' agreement, and a value less than .40 indicates 'poor' agreement [31]. The advantage of the kappa coefficient is that it is a measure of chance corrected concordance, meaning that it corrects the observed agreement for agreement that might occur by chance alone. There are difficulties with the interpretation of kappa and correlation coefficients that have been described by Feinstein and Brennan [,]. To examine the reliability coefficients calculated by the authors of MMT studies, see Table Table11.
Table 1
Characteristics of 10 studies of the intraexaminer and interexaminer reliability of manual muscle testing (RCTs indicated by **)
| Authors, date | Subjects | Examiners | Design | Findings and statistics |
| Pollard et al55 (2005) ** | 106 volunteers | Novice examiner (5th year) chiropractic student; experienced examiner (15 years MMT experience) | Interexaminer reliability of 2 common muscle tests | Deltoid muscle showed Cohen kappa value (k 0.62) and psoas muscle showed (k 0.67). Good interexaminer reliability shown between experienced and novice examiners. |
| Perry et al43 (2004) ** | 16 patients with post-polio syndrome; 18 patients without pathology; 26 patients with signs of hip extensor weakness and post-polio syndrome | Several examiners | Supine MMT of hip extensor strength compared to strength values obtained by traditional prone test of hip extensor muscles in patients with post-polio syndrome | Reliability testing showed excellent agreement (82%). Subjects with pathology had significant differences in mean muscle torque (P < .01) strength. Predictive validity of MMT in patients with symptomatic post-polio syndrome affecting hip extensor muscles was excellent. |
| Escolar et al56 (2001) | 12 children with muscular dystrophy | 12 novice and experienced examiners | To determine reliability of quantitative muscle testing (QMT, an instrument for measuring strength) compared to MMT | MMT was not as reliable among novice examiners as QMT. With adequate training of examiners an interclass correlation coefficient > 0.75 was achieved for MMT. |
| Caruso and Leisman 36 (2000) | 27 volunteers who knew nothing about MMT or AK | 2 examiners | To show the difference between 'weak' and 'strong' muscles, using MMT and dynamometer testing | Study showed that examiners with over 5 years experience using AK had reliability and reproducibility (98.2%) when their outcomes were compared. Perception of 'inhibition' or weakness made by examiner was corroborated by test pressure analysis using the dynamometer. |
| Florence et al 47 (1992) ** | 102 boys aged 5 to 15 years. | Physical therapists | A double-blind, multicenter trial to document the effects of prednisone on muscle strength in patients with Duchenne's muscular dystrophy (DMD). | Reliability of muscle strength grades obtained for individual muscle groups and of individual muscle strength grades was analyzed using Cohen's weighted Kappa. The reliability of grades for individual muscle groups ranged from .65 to .93, with the proximal muscles having the higher reliability values. The reliability of individual muscle strength grades ranged from .80 to .99, with those in the gravity-eliminated range scoring the highest. Concluded that the MMT was reliable for assessing muscle strength in boys with DMD when consecutive evaluations are performed by the same physical therapist. |
| Barr et al 42 (1991) | 36 boys (11.7 +/- 3.9 years) with Duchenne or Becker muscular dystrophy. | Upper and lower extremities were evaluated by MMT for function, range of motion, and strength. | The data were analyzed using intraclass correlation coefficients (ICCs). For the interevaluator phase, ICCs for MMT was .90; For the intraevaluator phase, corresponding ICC was .80 to .96. Results confirm and extend observations by others that these assessment measures are sufficiently reliable for use in multiinstitutional collaborative efforts. These results can be used to design clinical trials that have sufficient statistical power to detect changes in the rate of disease progression. | |
| Hsieh and Phillips 46 (1990) | 15 asymptomatic subjects | 3 chiropractors | To determine the reliability of manual dynamometry using AK style of MMT, comparing doctor-initiated and patient-initiated MMT | Intratester reliability and correlation coefficients for testers 1, 2, and 3 were 0.55, 0.75, and 0.76 with doctor-initiated method; 0.96, 0.99, and 0.97 when patient-initiated MMT method. The intertester reliability coefficients were 0.77 and 0.59 on day 1 and 2 respectively for doctor-initiated method; and 0.95 and 0.96 for the patient-initiated method. |
| Wadsworth et al 45 (1987) | 5 muscle groups on 11 patients | physical therapists | To compare the intrarater reliability of MMT and hand-held dynamometer tests | The correlation coefficients were high and significantly different from zero for four muscle groups tested dynametrically and for two muscle groups tested manually. The test-retest reliability coefficients for two muscle groups tested manually could not be calculated because the values between subjects were identical. Concluded that both MMT and dynamometry are reliable testing methods, given the conditions described in this study. |
| Florence et al 34 (1984) | Patients with Duchenne Muscular Dystrophy | physical therapists | To evaluate the (intraobserver) and (interobserver) reliability of MMT evaluation procedures to assess the efficacy of treatment of Duchenne muscular dystrophy. | Showed there was significant improvement in the degree of consistency of a given examiner's MMT scores when the examiner had more clinical experience and training in MMT. Author's concluded that MMT demonstrated reliability for an evaluation method that provided an objective foundation on which to claim if a drug or therapeutic procedure does or does not have an effect in treating Duchenne muscular dystrophy. |
| Jacobs 44(1981) | 65 patients with suspected thyroid dysfunction | 2 chiropractors | To compare AK diagnostic findings with laboratory findings | This double-blind study demonstrated an 81.9% agreement between two testers, indicating good inter-examiner reliability. |
This review of the literature shows the importance of clinical experience and expertise, and this factor has been highlighted in many papers discussing the reliability of the MMT [20-23,-]. The skills of the examiners conducting studies on MMT and their skills in interpreting the derived information will affect the usefulness of MMT data. The examiner is obliged to follow a standardized protocol that specifies patient position, the precise alignment of the muscle being tested, the direction of the resisting force applied to the patient, and the verbal instruction or demonstration to the patient. All of these precautions have proven necessary to reliably study the validity of the MMT in the diagnosis of patients with symptomatology.
There was significant improvement in the degree of consistency of a given examiner's scores (as noted by Florence et al 1984) [] when the examiner had more clinical experience and training in MMT. Mendell and Florence (1990) [], Caruso and Leisman (2000), [] and many other researchers of MMT have discussed the importance of considering the examiner's training on the outcomes of studies that assess strength via MMT [20-23].
Interexaminer reliability of the MMT has been reported by Lilienfeld et al (1954) [], Blair (1955)[], Iddings et al (1961) [], Silver et al (1970) [], Florence et al (1984) [], Frese et al (1987) [], Barr et al (1991) [] and Perry et al (2004) []. Test-retest reliability has been examined by Iddings et al (1961), [] Jacobs (1981) [44], Florence et al (1984) [], Wadsworth et al (1987) [], Mendell and Florence (1990) [], Hsieh and Phillips (1990) [], Barr et al (1991) [], Florence et al (1992) [], Lawson and Calderon (1997) [], Caruso and Leisman (2000) [], and Perry et al (2004) []. The levels of agreement attained, based upon +/- one grade were high, ranging from 82% to 97% agreement for interexaminer reliability and from 96% to 98% for test-retest reliability. The results of these studies indicate that in order to be confident that a true change in strength has occurred; MMT scores must change more than one full grade. In clinical research studies on chiropractic treatment, the change from an 'inhibited' or 'weak' muscle to a 'facilitated' or 'strong' muscle is a change in at least one full grade, and is a common result of successful treatment.
In the latter 11 studies, correlation coefficients are reported. These coefficients ranged from 0.63 to 0.98 for individual muscle groups, and from 0.57 to 1.0 for a total MMT score (comprised of the sum of individual muscle grades).
Using force measurements from both practitioner and patient, Leisman and Zenhausern demonstrated a significant difference in 'strong' versus 'weak' muscle testing outcomes and showed that these changes were not attributable to decreased or increased testing force from the practitioner performing the tests [].
Table Table11 provides a brief synopsis of several studies that investigated the reliability of MMT in both healthy and symptomatic subjects. The Table does not show the substantial amount of normative data that exists regarding muscle strength relating to patient age, position, tasks performed, and so on [51,52]. There also exists a large body of data demonstrating how electromyographic signals are used as an objective representation of neuromuscular activity in patients. The EMG is a valid index of motor unit recruitment and reflects the extent to which the muscle is active; however there are some difficulties with the sensitivity and specificity of electrodiagnosis []. All of these studies using MMT and instrumentation have collectively made a significant contribution to the study of neuromuscular function and represent different aspects of the muscular activity going on in patients.
Research On the Validity of MMT
The next section of Results looks at the relationship between muscle strength as measured by MMT findings and the functional status of patients with a variety of symptoms.
Validity is defined as the degree to which a meaningful interpretation can be inferred from a measurement or test. Payton (1994) [58] states that validity refers to the appropriateness, truthfulness, authenticity, or effectiveness of an observation or measurement. In examining research studies and examination techniques using MMT and spinal manipulative therapy (SMT), clinicians need to become familiar with several different types of validity.
Construct and content validity of MMT
Construct and content validity are two types of theoretical or conceptual validity. Generally, construct and content validity are proven through logical argument rather than experimental study. Construct validity is the theoretical foundation on which all other types of validity depend. Construct validity attempts to answer the questions, 'Can I use this measurement to make a specific inference?' and 'What does the result of this test mean?'
From the original work of Lovett (1915) [25,26] who developed MMT as a method to determine muscle weakness in polio patients with damage to anterior horn cells in the spinal cord, to the measurement of physical weakness from faulty and painful postural conditions, injuries, and congenital deformities [20-23,59,60], to neurologists who adopted MMT as part of their physical diagnostic skills, [24] to the use of MMT by some chiropractors beginning with AK technique to diagnose structural, chemical, and mental dysfunctions, the concept of manually examining the nervous system's status through MMT continues to evolve and gain adherents to this method [61]. The validity of Lovett's original MMT methods was based on the theoretical construct that properly innervated muscles could generate greater tension than the partially innervated muscles present in patients with anterior horn cell damage.
AK extends Lovett's construct and theorizes that physical, chemical, and mental/emotional disturbances are associated with secondary muscle dysfunction affecting the anterior horn of the spinal cord – specifically producing a muscle inhibition (often followed by overfacilitation of an opposing muscle and producing postural distortions in patients). Goodheart suggested, contrary to the physiotherapeutic understanding of the time, that muscle spasm was not the major initiator of structural imbalance [,6]. According to Goodheart, the primary cause of structural imbalance is muscle weakness. Goodheart theorized that the primary weakness of the antagonist to the spastic muscle to be the problem. Muscle weakness (as observed by MMT) is understood as an inhibition of motor neurons located in the spinal cord's anterior horn motor neuron pool [].
Chiropractic AK research has also suggested that there are five factors or systems to consider in the evaluation of muscle function: the nervous system, the lymphatic system, the blood vascular system, cerebrospinal fluid flow, and the acupuncture system [,6].
Lamb states (1985) that MMT has content validity because the test construction is based on known physiologic, anatomic and kinesiologic principles [63]. A number of research papers have dealt with this specific aspect of MMT in the diagnosis of patients [,].
There have been a number of papers that have specifically described the validity of MMT in relationship to patients with low back pain. The correlation between 'inhibited' or 'weak' MMT findings and low back pain has been well established in the research literature. Several papers have shown that MMT is relevant and can be employed in a reliable way for patients with low back pain [63,]. In a paper by Panjabi, it is proposed that the function of muscles, as both a cause and a consequence of mechanoreceptor dysfunction in chronic back pain patients, should be placed at the center of a sequence of events that ultimately results in back pain []. This paper argues that as a result of spinal dysfunctions (articular dysfunction, spinal lesions, and somatic dysfunction are terms also employed), muscle coordination and individual muscle force characteristics are disrupted, i.e. inhibited muscles on MMT. The injured mechanoreceptors generate corrupted transducer signals (that research suggests may be detected by EMG, dynamometers, and MMT), which lead to corrupted muscle response patterns produced by the neuromuscular control unit.
This article may be important for those in the manipulative professions who are evaluating the existence and consequences of spinal dysfunction. The key technical factor in this hypothesis would be the MMT that makes the detection of the muscular imbalances and spinal dysfunction cited by Panjabi identifiable. Another paper by Hodges et al (2003) suggests this hypothesis also []. Pickar has also shown there is a substantial experimental body of evidence indicating that spinal manipulation impacts primary afferent neurons from paraspinal tissues, immediately effecting the motor control system and pain processing [].
Lund et al (1991) [] reviewed articles describing motor function in five chronic musculoskeletal pain conditions (temporomandibular disorders, muscle tension headache, fibromyalgia, chronic lower back pain, and post-exercise muscle soreness). Their review concluded that the data did not support the commonly held view that some form of tonic muscular hyperactivity maintains the pain of these conditions. Instead, they maintain that in these conditions the activity of agonist muscles is often reduced by pain, even if this does not arise from the muscle itself. On the other hand, pain causes small increases in the level of activity of the antagonist. As a consequence of these changes, force production and the range and velocity of movement of the affected body part are thought to be reduced.
This paper describes with fascinating similarity one of the major hypotheses in MMT and chiropractic, namely that physical imbalances produce secondary muscle dysfunction, specifically a muscle inhibition (usually followed by overfacilitation of an opposing muscle). A paper by Falla et al (2004) described a similar model but involving patients with chronic neck pain []. A paper by Mellor et al (2005) presented this model in relationship to anterior knee pain [], and Cowan et al (2004) in relationship to chronic groin pain with another paper demonstrating this mechanism in patellofemoral pain syndrome [,].
According to several studies, patients with low-back pain have lower mean trunk strength than asymptomatic subjects (Nummi et al 1978, Addison & Schultz 1980, Karvonen et al 1980, MacNeill et al 1980, Nordgren et al 1980, Mayer et al 1985, Triano 1987, Rantanen et al 1993, Hides et al 1996, Hodges et al 1996) [-]. Lifting strength is also decreased in persons disabled with chronic low-back pain (Chaffin & Park, 1973, Biering-Sorensen 1984, Mayer et al 1988) [-]. Pain itself is possibly a strength-reducing factor, as is the duration of back pain (Nachemson & Lindh 1969) [].
These studies do not always clarify whether a muscle weakness or imbalance is primary or secondary to low-back pain. In spite of this, muscle weakness has frequently been cited as a primary factor in the etiology of low-back pain. (See Table Table2)2) This is one of the bases on which Lamb argues that MMT has content validity [63].
Table 2
Characteristics of 8 Studies showing the prevalence of muscle dysfunction in patients with back pain (RCTs indicated by **)
| Authors, date | Subjects | Design | Findings and statistics |
| Hossain et al 90 (2005) | Literature review | Gait analysis studies reviewed show an orderly sequence of muscle activation – this contributes to efficient stabilization of the joint and effective weight transfer to the lower limb. Gluteus maximus fibres – lying almost perpendicular to the joint surfaces are oriented for this purpose. Biceps femoris is another important muscle that can also influence joint stability by its proximal attachment to sacrotuberous ligament. | Altered pattern of muscle recruitment has been observed in patients with low back pain. Because of its position as a key linkage in transmission of weight from the upper limbs to the lower, poor joint stability could have major consequences on weight bearing. It is proposed that sacro-iliac joint dysfunction can result from malrecruitment of gluteus maximus motor units during weight bearing, resulting in compensatory biceps femoris over activation. The resulting soft tissue strain and joint instability may manifest itself in low back pain. This thesis was also proposed by Janda (1964). 18 |
| Falla et al 71 (2004) ** | 10 patients with chronic neck pain; 10 controls | To compare activity of deep and superficial cervical flexor muscles during a test of craniocervical flexion. | Showed a strong linear relation between the electromyographic amplitude of the deep cervical flexor muscles and the incremental stages of the craniocervical flexion test for control and individuals with neck pain (P = 0.002). A reduced performance of the craniocervical flexion test is associated with dysfunction of the deep cervical flexor muscles. |
| Hodges et al 83 (1996) ** | 15 patients with low back pain and 15 matched control subjects | Subjects performed rapid shoulder flexion, abduction, and extension in response to a visual stimulus. Electromyographic activity of the abdominal, and lumbar multifidus muscles recorded by surface electrodes. | Contraction of transversus abdominis was significantly delayed in patients with low back pain with all movements. The delayed onset of contraction of transversus abdominis indicated a deficit of motor control and is hypothesized to result in inefficient muscular stabilization of the spine. |
| Triano et al 91 (1987) ** | 41 low-back pain patients; and 7 pain-free control subjects | To examine relations among some objective and subjective measures of low-back-related disability | Oswestry disability score related significantly (P less than 0.001) to presence or absence of relaxation in back muscles during flexion. Mean trunk strength ratios were inversely related to disability score (P less than .05). Findings imply that myoelectric signal levels, trunk strength ratios, and ranges of trunk motion may be used as objective indicators of low-back pain disability. |
| Biering-Sorensen 85(1984) | 449 men and 479 women | The examination consisted of anthropometric measurements, flexibility/elasticity measurements of the back and hamstrings, as well as tests for trunk muscle strength and endurance. | The main findings were that good isometric endurance of the back muscles may prevent first-time occurrence of low back trouble (LBT) in men and that men with hypermobile backs are more liable to contract LBT. Weak trunk muscles and reduced flexibility/elasticity of the back and hamstrings were found as residual signs, in particular, among those with recurrence or persistence of LBT in the follow-up year. |
| McNeill T et al 92 (1980) ** | 27 healthy males and 30 healthy females; and 25 male and 15 female patients with low-back pain and/or sciatica. | Maximum voluntary isometric strengths were measured during attempted flexion, extension, and lateral bending from an upright standing position. | The ratios showed that the patients with low back pain and/or sciatica had extension strengths that were significantly less than their strengths in the other types of movements tested. The strength ratios for attempted extension were particularly low for patients with sciatica. Both male and female with LBP and/or sciatica had approximately 60% of the absolute trunk strengths of the corresponding healthy subjects. |
| Karvonen et al 77 (1980) | 183 male conscripts. A history of sciatica was reported by 8%, lumbago by 13%, back injury by 13% and low back insufficiency by 63%. | To correlate muscle weaknesses in young men with complaints of LBP | Weak trunk extensors were associated with a history of sciatica; weak trunk flexors with back injuries and with current backache at work/exercise. Weak leg extensors showed associations with a history of low back insufficiency and of sick leave due to the back and with current hip pain. Men with a history of lumbago and of hip and knee complaints performed poorly during 12 min of running. The questionnaire and strength measurements proved suitable for studying low back syndrome in its early stages. |
| Addison et al 76 (1980) | 16 male and 17 female patients with chronic LBP | Maximum voluntary trunk strengths in the standing position were measured during attempted flexion, extension, and lateral bending. The trunk strengths of these patients were then compared with those of healthy subjects and with those of patients with low-back disorders who sought treatment as outpatients of a general orthopaedic office practice. | When compared with healthy subjects, the patients seeking hospitalization had significantly smaller strengths during attempted extension relative to their strengths during attempted flexion or lateral bending. |
A number of general MMTs have been employed by all primary contact practitioners for the examination of patients with sciatic neuralgia. Dorsiflexion of the foot and the great toe, plantar flexion of the foot and great toe, quadriceps weakness, and peroneal muscle tests are each indicative of the status of the sciatic nerve and its branches [88,].
To test the construct validity of these original hypotheses, researchers have attempted to quantify the muscle weakness that occurs with specific clinical conditions such as low back pain and soft tissue injuries. (See Table Table22)
The Convergent and Discriminant Validity of MMT
Convergent validity exists when a test, as predicted, demonstrates a strong correlation between two variables. Discriminant validity exists when the test, as predicted, demonstrates a low correlation between two variables. These tests, when found to have the proper correlations, lend support to the construct validity of the method of testing.
The convergent and discriminant validity of MMT was examined in a study by Jepsen et al (2006) []. They examined the relationship between MMT findings in patients with and without upper limb complaints. The examiners were blinded as to patient-related information, and examined 14 muscles in terms of normal or reduced strength. With a median odds ratio of 4.0 (95%CI, 2.5–7.7), reduced strength was significantly associated with the presence of symptoms.
Perry et al (2004) showed excellent convergent and discriminant validity of MMT in 16 patients with and 18 patients without post-polio syndrome pathology. Subjects with pathology showed significant differences in mean muscle strength (P < 0.01). The predictive validity of MMT in patients with symptomatic post-polio syndrome affecting the hip extensor muscles was found to be excellent [].
Pollard et al (2006) also studied the convergent and discriminant validity of MMT in order to determine if a positive correlation of therapy localization to the 'ileocecal valve point' producing weakness on MMT could predict low back pain in patients with and without low back pain [54]. The study also aimed to determine the sensitivity and specificity of the procedure. Of 67 subjects who reported low back pain, 58 (86.6%) reported a positive test of both low back pain and ICV point test. Of 33 subjects, 32 (97%) with no back pain positively reported no response to the ICV point test. Nine (9) subjects (13.4%) reported false negative ICV tests and low back pain, and 1 subject (3%) reported a false positive response for ICV test and no low back pain. Their results demonstrated that the low back pain group had significantly greater positive results (inhibited MMT) than those of the pain free group. Assuming this study is sound it may demonstrate the convergent validity of the method of MMT in relationship to patients with low back pain. The discriminant validity of MMT was shown in this study by its ability to find a low number of positive test results in the pain free groups. However, before accepting these results it would be important for them to be reproduced in another study.
Studies like the ones described above and later in this review (that examine whether MMT can discriminate between abnormal and normal spinal function and pain states) contribute to the evidence available to clinicians supporting the validity of MMT.
Concurrent Validity of MMT
The concurrent validity of MMT has also been examined in several studies comparing strength scores obtained by MMT with strength readings obtained using quantitative instruments. The concurrent validity of a test refers to a test's ability to produce similar results when compared to a similar test that has established validity. The concurrent validity of the MMT would be examined when the MMT is compared to a 'gold standard' confirmation diagnosis using EMG and/or dynamometer testing, for instance. Many studies have compared the findings of MMT with dynamometer tests favorably. (See Table Table33)
Table 3
Characteristics of 8 studies examining the concurrent validity of MMT
| Authors, date | Subjects | Examiners | Design | Findings and statistics |
| Bohannon 95 (2001) | 128 acute knee rehabilitation patients | physical therapist | To compare MMT with hand-held dynamometer measurements of knee extension strength | MMT and dynamometer scores highly correlated (r = 0.768; P < 0.001). Convergent and construct validity of MMT and dynamometry measurements demonstrated. |
| Caruso and Leisman36 (2000) | 27 volunteers with no knowledge about MMT or AK | 2 examiners | To show the difference between 'weak' and 'strong' muscles, using MMT and dynamometer testing | Study showed that examiners with over 5 years experience using AK had reliability and reproducibility when their outcomes were compared. Perception of 'inhibition' or weakness made by examiner was corroborated by test pressure analysis using the dynamometer. |
| Lawson and Calderon 48 (1997) ** | 30 asymptomatic volunteers | Medical doctor | 10 upper extremity muscles were tested using AK methods in double-blind conditions. | MMTs of 'weak' or 'strong' muscles showed significantly different electromyographic measurements and demonstrated a high correlation between testing methods. |
| Schwartz et al 96 (1992) | 122 patients with spinal cord injuries at C4–C6 | physical therapists | Relationship between MMT and hand-head myometry compared | Sequential examinations with MMT and myometry were made at 72 hours, 1 week, and 2 weeks post-spinal cord injury and at 1, 2, 3, 4, 6, 12, 18, and 24 months post-injury. Results showed that 22 of 24 correlations between MMT and myometry were significant at p values less than .001. |
| Perot et al 57 (1991) | 10 subjects | Chiropractors | To measure and compare both electromyographic and MMT results after proprioceptive techniques to both strengthen and weaken muscles | Response of tibialis anterior muscle to proprioceptive technique showed a significant EMG difference that corresponded to the difference found between 'strong' and 'weak' MMT outcomes. AK proprioceptive procedure to reduce muscle tone found to correlate with MMT outcomes. |
| Hsieh and Phillips 46 (1990) | 15 asymptomatic subjects | 3 chiropractors | To determine the concurrent validity of manual dynamometry using AK style of MMT, comparing doctor-initiated and patient-initiated MMT | Intratester reliability and correlation coefficients for testers 1, 2, and 3 were 0.55, 0.75, and 0.76 with doctor-initiated method; 0.96, 0.99, and 0.97 when patient-initiated MMT method. The intertester reliability coefficients were 0.77 and 0.59 on day 1 and 2 respectively for doctor-initiated method; and 0.95 and 0.96 for the patient-initiated method. |
| Wadsworth et al 45 (1987) | 5 muscle groups on 11 patients | physical therapist | To compare the concurrent reliability of MMT and hand-held dynamometer tests | The correlation coefficients were high and significantly different from zero for four muscle groups tested dynametrically and for two muscle groups tested manually. The test-retest reliability coefficients for two muscle groups tested manually could not be calculated because the values between subjects were identical. Conclusion that both MMT and dynamometry are reliable testing methods, given the conditions described in this study. |
| Bohannon 97 (1986) | 50 patients | physical therapist | To determine the relationship between MMT word scores and dynamometer force scores using Kendall tau. | MMT scores and dynamometer test scores were significantly correlated (p less than 0.001). Percentage MMT and dynamometer test scores were significantly different (p less than 0.001). These results suggest that the two procedures measure the same variable-strength. |
| Marino et al 50 (1982) | 128 patients | physical therapists | To compare MMT findings with hand-held dynamometer (HHD) findings, with precise repetition of the MMT | The MMT and HHD values were within 5% of each other. The average hip abduction and hip flexion scores measured by the HHD were consistent with the examiner's perception of muscle weakness (P less than 0.001). |
| Triano and Davis 98 (1976) | 10 patients with 'reactive muscle' phenomena described in AK | chiropractor | In patients with reactive muscle pairs (between the rhomboid and deltoid muscles), EMG and MMT findings were compared. | Study demonstrated that the reactive muscle phenomenon is, in fact, a physiologic imbalance of muscle measurable by EMG and MMT and was not a psychologic suggestion or an overpowering of the tested arm by brute force. These data showed that the deltoid-rhomboid 'reactive muscle' represents a real physiological phenomenon. |
Marino et al (1982) [] and Wadsworth et al (1987) [] showed significant reliability between handheld dynamometers and MMT. Scores measured with the dynamometers were consistent with the examiner's perception of muscle weakness (P less than 0.001) in both studies.
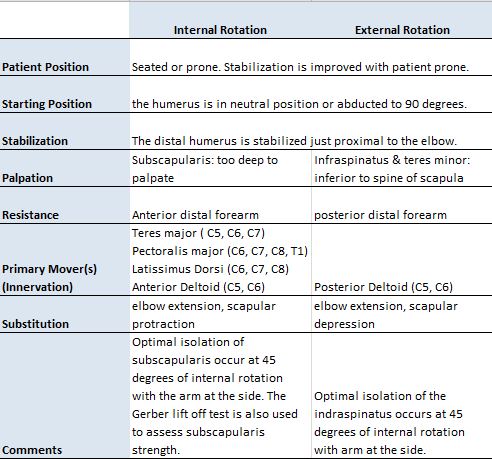
Manual Muscle Testing Shoulder External Rotation
Leisman et al (1995) showed that chiropractic muscle testing procedures could be objectively evaluated through quantification of the electrical characteristics of muscles, and that the course of chiropractic treatments can be objectively plotted over time [].
The use of EMG or dynamometers as a gold standard is arguable however because false positive or negative findings may exist, and these instruments measure different aspects of muscular activity [20]. Even the MRI (another diagnostic 'gold standard') has been found to lack sensitivity and specificity. MRI can identify a lesion but cannot detail the relationship of the finding with the patient's symptoms [94].
There is increasing demand for objectivity in regard to muscle testing measurements. Electromyograms are expensive machines, and setting patients up on the machines in the clinical setting is time-consuming. A review of the literature on dynamometers reveals some of the problems associated with their use. These include problems with the actual forces measured by a hand-held dynamometer (HHD); providing the stabilization that is essential for controlling variables and for standardization of the testing technique; as even a slight tipping of the devise during testing can alter its results [20-22,]. These are important factors when considering the cost-effectiveness and clinical usefulness of these other testing procedures for muscle strength assessment.
Predictive Validity and Accuracy of the MMT
A second form of validity is called predictive validity. Comparing a test to supporting evidence that is obtained at a later date assesses predictive validity.
The accuracy of a diagnostic test is usually determined by examining the ability of the test to assist clinicians in making a correct diagnosis. A good diagnostic test minimizes the probability of the clinician finding a positive response in healthy people and negative test results in people with dysfunction or pathology. A good diagnostic test therefore minimizes the probability of either a false positive or a false negative result. The accuracy of the test is defined as the probability that people who truly should have the positive response receive a positive response when the test is performed. The accuracy of the test is also defined as the probability that people who should truly have a negative response correctly receive a negative response when the test is performed.
Table Table44 provides a brief summary of several studies that examine the presence of positive MMT in suspected disorders of neural origin.
Table 4
Characteristics of 14 studies examining the Clinical Relevance, Predictive Validity and Accuracy of MMT (RCTs indicated by **)
| Authors, date | Diagnosis | Subjects | Repeated Observations | Treatments | Outcomes |
| Jepsen et al 93 (2006) ** | Upper limb pain | 41 patients, 19 with upper limb pain | MMT, with examiners blinded as to patient pain status. | None | Reduced strength of upper limb muscles was significantly associated with the presence of symptoms. A median odds ratio of 4.0 (2.5–7.7). |
| Pollard et al 54 (2006) ** | Low back pain | 67 of 100 patients have low back pain | MMT with therapy localization to an Ileo-cecal valve reflex point | None | Of 67 subjects who reported low back pain, 58 (86.6%) reported a positive test of both low back pain and ICV point test. Of 33 subjects, 32 (97%) with no back pain positively reported no response to ICV point test. Nine (9) subjects (13.4%) reported false negative ICV tests and low back pain, and 1 subject (3%) reported a false positive response for ICV test and no low back pain. The ileocecal valve test as a diagnostic measure of low back pain was found to have excellent measures of sensitivity, specificity and diagnostic competency. |
| Niemuth et al 99 (2005) ** | Single leg overuse injury | 30 recreational injured runners (17 female, 13 male) and 30 noninjured runners (16 female, 14 male) served as controls. | Muscle strength of the 6 major muscle groups of the hip was recorded using a hand-held dynamometer. | None | No significant side-to-side differences in hip group muscle strength were found in the noninjured runners (P = 0.62–0.93). Among the injured runners, the injured side hip abductor (P = 0.0003) and flexor muscle groups (P = 0.026) were significantly weaker than the noninjured side. In addition, the injured side hip adductor muscle group was significantly stronger (P = 0.010) than the noninjured side. |
| Michener et al 64 (2005) | Shoulder pain | 40 patients with shoulder pain and functional loss | Hand held dynamometer testing performed as MMT for the lower trapezius, upper trapezius, middle trapezius, and serratus anterior muscles. Concurrently, surface electromyography (sEMG) data were collected for the 4 muscles. The same procedures were performed 24 to 72 hours after the initial testing by the same tester. | None | Intraclass correlation coefficients for intratester reliability of measurements of isometric force obtained using an HHD ranged from .89 to .96. The standard error of the measure (90% confidence interval [CI]) ranged from 1.3 to 2.7 kg; the minimal detectable change (90% CI) ranged from 1.8 to 3.6 kg. Construct validity assessment, done by comparing the amounts of isometric muscle activity (sEMG) for each muscle across the 4 muscle tests, revealed that the muscle activity of the upper trapezius and lower trapezius muscles was highest during their respective tests. |
| Moncayo et al 100 (2004) | Thyroid associated orbitopathy (TAO) | 32 patients with TAO, 23 with a long-standing disease, and 9 showing discrete initial changes | Positive TL (patient touches area of dysfunction and weakening occurs on MMT) reactions were found in the submandibular tonsillar structures, the tonsilla pharyngea, the San Yin Jiao point, the lacrimal gland, and with the functional ocular lock test of AK. | AK treatment and homeo-pathic remedies | Change of lid swelling, of ocular movement discomfort, ocular lock, tonsil reactivity and Traditional Chinese Medicine criteria including tenderness of San Yin Jiao (SP6) and tongue diagnosis were improved. Clinical trial of 3–6 months showed all relevant parameters improved. |
| Rainville et al 101 (2003) | sciatica | 33 patients with L3 or L4 radiculopathy; 10 patients with L5 or S1 radiculopathy | To test quadriceps strength with MMT | None | Knee flexed MMT weakness of the quadriceps showed kappa coefficient of (0.66). Patients with radicular pain caused by L5 or S1 could perform the quadriceps test. Weakness of quadriceps correlated with L3 or L4 radiculopathy. |
| Great Lakes ALS Study Group 65 (2003) | amyotrophic lateral sclerosis (ALS) | 63 patients with ALS | Compared test reliability of MMT and maximal voluntary isometric contraction (MVIC) scores among institutions and test validity by comparing change over time between MMT and MVIC. | None | Reproducibility between MVIC and MMT was equivalent. Sensitivity to detect progressive weakness and power to detect this change, however, favored MMT. In multicentered trials, uniformly trained physical therapists reproducibly and accurately measure strength by both MMT and MVIC. The authors found MMT to be the preferred measure of global strength because of its better Pearson correlation coefficients, essentially equivalent reproducibility, and more favorable coefficient of variation. |
| Nadler et al 66 (2001) | 13 college athletes with low back pain | Of 163 athletes (100 male, 63 female), 5 of 63 females and 8 of 100 males required treatment for LBP. | A dynamometer incorporated into a specially designed anchoring station was used for testing the hip extensors and abductors. The maximum force generated for the hip abductors and extensors was used to calculate a percentage difference between the right and left hip extensors and abductors. | athletic trainers for LBP unrelated to blunt trauma over the ensuing year | Logistic regression analysis indicated that for female athletes, the percentage difference between the right and left hip extensors was predictive of whether treatment for LBP was required over the ensuing year (P = 0.05). Validity shown that hip muscle imbalance is associated with LBP occurrence in female athletes. Research supports the need for the assessment and treatment of hip muscle imbalance in individuals with LBP. |
| Monti et al 103 (1999) | None | 89 healthy college students | To determine the differences in MMT outcomes after exposure to congruent and incongruent semantic stimuli | None | Approximately 17% more total force over a 59% longer period of time could be endured when subjects repeated semantically congruent statements (p < .001). Over all, significant differences were found in muscle test responses between congruent and incongruent semantic stimuli. |
| Schmitt et al 104 (1998) | Allergies | 17 subjects | To determine whether subjective muscle testing employed by Applied Kinesiology practitioners, prospectively determine those individuals with specific hyperallergenic responses. | None | Each subject showed muscle-weakening (inhibition) reactions to oral provocative testing of one or two foods for a total of 21 positive food reactions. Tests for a hypersensitivity reaction of the serum were performed using both a radio-allergosorbent test (RAST) and immune complex test for IgE and IgG against all 21 of the foods that tested positive with A.K. muscle screening procedures. These serum tests confirmed 19 of the 21 food allergies (90.5%) suspected based on the applied kinesiology screening procedures. |
| Goodheart 105 (1990) | Imbalanced weight bearing on right and left feet | 40 patients | 40 patients were evaluated for pre- and post-treatment weight balance. | AK examin-ation and treatment | Of the 40 patients, only one had minimal changes in weight upon two scales beneath the feet when both flexing and extending the spine. |
| Jacobs et al 44 (1984) | Thyroid dysfunction | 65 patients | Patients evaluated for thyroid dysfunction by MMT, and laboratory testing. | AK and labor-atory examina-tion | MMT ratings correlated with clinical ratings (rs = .36, p < 0.002) and with laboratory ratings (rs = .32, p < 0.005). Correlation between clinical and laboratory diagnosis was .47, p < 0.000. Three AK TL points had a significant correlation with the laboratory diagnosis (p < .05). 'AK enhanced but did not replace clinical/laboratory diagnosis of thyroid dysfunction.' |
| Scoop 106 (1979) | Allergy | 10 subjects | Subjects with unilateral weak muscles were given either a placebo or the nutrient that is hypothesized in AK to be associated with the muscle. Muscle tone was measured by a Jaymar dynamometer and with AK MMT methods. | Nutrition | The increase in muscle tone approximately 10 seconds after ingestion was 21% for the nutrient group and was a statistically significant (p < 0.05) increase in comparison with the placebo group. In the cerebral allergy testing part of the study, a 15% decrease in muscle tone of the pectoralis major clavicular was used as the criterion for cerebral allergy. The muscle testing method was then compared to results obtained by a Philpott-type fast with progressive reintroduction of foods. Correlation between foods identified as provocative by muscle testing and by the fast was .81. Observation of clinical results obtained with muscle testing suggests the method has substantial clinical utility. Pearson Product-Moment Correlation between testers was .91, suggesting that muscle testing is reliable between testers. |
| Carpenter et al 107 (1977) | None | 80 students | The muscles hypothesized in AK to be associated with certain organs were tested with an instrument after irritation of the related organs. Then a control muscle was tested. 4 organ muscle associations were evaluated: the eye, ear, stomach, and lung. The stomach was irritated by placing cold water into it; the eye with chlorinated water; the ear with sound of a controlled frequency and decibel rate; and the lung with cigarette smoke. | None | In 80 subjects, a total of 139 organs were irritated. In all cases, the associated muscle weakened significantly after the irritation. The control muscle also weakened, but to a much lesser degree. |
The Emerging Construct in the Research on MMT
In order to evaluate the scientific merit of MMT we have discussed the importance of the operational definitions, reliability and validity in MMT research. The original construct of the MMT was that it documented impairments in muscle strength. Muscle inhibitions (detected by MMT) are understood in chiropractic and AK to be reflective of an inhibition of motor neurons located in the spinal cord's anterior horn motor neuron pool as a result of dysfunction involving one or more of the '5-factors of the IVF' [-9,].
A complication to the original construct of MMT from Lovett and others has emerged with the increasing awareness that the responses to the MMT are not solely due to the denervation effects on neural tissues in conditions like polio, but also co-existing inputs to the spinal cord's anterior horn and the processing state of the CNS []. Chiropractic research and anecdotal evidence from clinical practice have also suggested that there are five factors or systems to consider in the evaluation of muscle function: the nervous system, the lymphatic system, the vascular system, cerebrospinal fluid flow, and the acupuncture system [-9,]. Chiropractic clinical experience and research has also suggested that dysfunction in a muscle may be caused by a failure of any of these systems and that the MMT response may provide important clues regarding the origin of that dysfunction. Applying the proper manipulative therapy may then result in improvement in the inhibited muscle, pain, movement and posture. (See Table Table5)5) However RCTs and other substantive research studies are required before we can assert with confidence the relevance of each of these factors.
Table 5
Characteristics of 19 case reports of positive experiences for patients (n = 1 – 88) treated with chiropractic AK technique
| Authors, date | Diagnosis | Subjects | Repeated Observations | Treatments | Outcomes |
| Cuthbert 109 (2006) | Motion sickness disorder | 1: 66 yoa female 2: 45 yoa female 3: 9 yoa female | Proprioceptive testing (Freeman-Wyke and Hautant's tests), AK MMT and palpation | Spinal and cranial chiropractic manipulative therapy (CMT) | 1: Able to drive car and ride in a boat and airplane symptom free after 4 visits. 2: Able to drive car symptom free after 6 visits. 3: Able to drive in car symptom free after 4 visits |
| Cuthbert et al 110 (2005) | optic nerve neuritis exacerbated by an Arnold-Chiari malformation (Type I) of the cerebellum | 1: 20 yoa female | AK MMT to diagnose vertebral subluxations and cranial lesions; ocular muscle testing, TMJ testing | Cranial and spinal CMT | Patient had lost her vision in the right eye 3 weeks previous to treatment. After 1 visit, patient could see 20–30 on Snellen eye chart. Visual acuity 20-13 after 3rd visit and asymptomatic 3 years later. |
| Meldener 111 (2005) | Post-surgical hip dislocation | 1: 75 yoa male | AK MMT to diagnose muscular weakness around hip and throughout the body | AK and CMT therapy, focusing on the connection of the TMJ and occlusion to instability of the hip | No hip dislocation since vertical dimension was increased with new upper dentures on doctor's recommendation. |
| Chung et al 112 (2005) | Dental occlusion problems | 7: male 3: female | AK MMT during application of an oral dental appliance | None | AK MMT reliable and repeatable on different days. MMT useful to locate the kinesiologic occlusal position for the fabrication of an oral appliance to treat TMJ disorders. |
| Caso 113 (2004) | congenital bowel abnormality related to low back pain. | 1: 29 yoa male | AK MMT to diagnose large bowel dysfunction | CMT and stimulation of Chapman's reflex points by the doctor and the patient at home | Resolution of the patient's low back pain as well as improved bowel function. |
| Moncayo et al 100 (2004) | Thyroid associated orbitopathy (TAO) | 32 patients with TAO, 23 with a long-standing disease, and 9 showing discrete initial changes | Positive TL (patient touches area of dysfunction and weakening occurs on MMT) reactions were found in the submandibular tonsillar structures, the tonsilla pharyngea, the San Yin Jiao point, the lacrimal gland, and with the ocular lock test of AK. | AK treatment and homeopathic remedies | Change of lid swelling, of ocular movement discomfort, ocular lock, tonsil reactivity and Traditional Chinese Medicine criteria including tenderness of San Yin Jiao (SP6) and tongue diagnosis were improved. Clinical trial of 3–6 months showed all relevant parameters improved. |
| Cuthbert 114(2003) | Down syndrome | 15 children | Informal report by the parents of child's function and health status. | CMT to the spine and cranium, with nutritional support as needed. | Improved fine motor skills; use of the hands and fingers; ability to crawl bilaterally with arms and legs; ability to stand and walk; decrease in tongue thrusting; problems with ears and sinuses were all improved in function as noted by parents, teachers, and doctor. |
| Maykel 115 (2003) | Blocked naso-lacrimal canal | 1: 14-month male | AK MMT and informal report of child's function and health status by the parents. | CMT to the spine and cranium | Child treated 5 times over a 6-week period with resolution of his eye problem. |
| Weiss 116 (2003) | Menstrual difficulty and exhaustion | 1: 39 yoa female | AK MMT and patient report of condition | Nutritional counseling and CMT to the spine and cranium | Treatment to the sacrococcygeal area with cranial correction and nutritional support improved her energy level and cycling performance. |
| Sprieser 117 (2002) | Episodic paroxysmal vertigo | 1: 17 yoa female | AK MMT and patient report of her condition | CMT to the spine and cranium as well as AK/meridian therapy techniques | After 4 treatments and 3 other treatments by a Qi-Gong master the patient remained free of any vertigo at 3 year follow up. |
| Leaf 118 (2002) | Severe equilibrium problems | 1: 48 yoa female | AK MMT and patient report of condition | Cervical traction of 6 pounds while patient walked for 15 minutes | After cervical traction-distraction patient was able to stand with her feet together with no body sway and displayed no signs of nystagmus. |
| Gregory et al 119 (2001) | women with moderate to severe breast pain | 88: females, predominantly premenopausal, with cyclical and non-cyclical breast pain | AK MMT to diagnose neurolymphatic reflex dysfunction of the large intestine | CMT and stimulation of Chapman's reflex points by the doctor and the patient at home | Immediately after treatment there was considerable reduction in breast pain in 60% of patients with complete resolution in 18%. 2 months after initial treatment, there was a reduction in severity, duration and frequency of pain of 50% or more in 60% of cases (P < 0.01). |
| Cuthbert 120 (2001) | Bell's Palsy | 1: female | AK MMT to diagnose cranial, cervical, TMJ, and muscular imbalances | CMT to the spine, TMJ, and cranium | Complete resolution of facial nerve palsy after 6 visits over 14 days. |
| Calhoon 121 (2001) | Multiple sclerosis | 1: 43 yoa female | AK MMT and patient report of condition | CMT to the spine, TMJ, and cranium and nutritional support | 26 months after initial visit patient had regained her ability to write and could shower without assistance for the first time in 2 years. |
| Mathews et al 122 (1999) ** | Learning disabilities | 10 children compared with a control group of 10 children matched for age, IQ and social background that had not received any treatment over a similar period. | AK MMT examination and sensory challenges; the children were tested before and after treatment by an Educational Psychologist using standardized tests of intelligence to monitor changes in their learning skills. | AK treatment | Educational psychologist's testing demonstrated children treated with AK had an improvement in their learning abilities during the course of 9 to 12 treatment sessions during a period of 6–12 months. |
| Masarsky et al 123 (1991) | Somatic dyspnea | 6: males and females | AK MMT examination methods; forced vital capacity (FVC) and forced expiratory volume in one second (FEV-1) measurements pre- and post-treatment (post-treatment measurements taken 3 days later to 1 month later). | AK treatment including neurolymphatic and neurovascular reflexes were employed for the diaphragm muscle; evaluation of the meridian system; cranial manipulation (AK methods); and treatment for inhibited muscles involved in respiration. | All patients reported improvement in their breathing difficulty. 4 of the 6 patients also had improved FCV and FEV-1 between 0.1 and 0.8 liters. |
| Goodheart 105 (1990) | Imbalanced weight bearing on right and left feet | 40 patients | 40 patients were evaluated for pre- and post-treatment weight balance. | AK examination and treatment | Of the 40 patients, only one had minimal changes in weight upon two scales beneath the feet when both flexing and extending the spine. |
| Masarsky et al 124 | Chronic obstructive pulmonary disease | 1: male | AK MMT examination methods; forced vital capacity (FVC) and forced expiratory volume in one second (FEV-1) measurements pre- and post-treatment, covering an 8-month period. | AK examination and treatment | Improvements were noted in forced vital capacity, forced expiratory volume in one second, coughing, fatigue, and ease of breathing (sign significant at 0.005 level). Improvement was also noted in laryngospasm. |
| Jacobs et al 44 (1984) | Thyroid dysfunction | 65: males and females | Patients evaluated for thyroid dysfunction by AK and laboratory testing | None | AK ratings correlated with laboratory ratings (rs = .32, p < .002) and with laboratory ratings (rs = .32, p < .005). Correlation between clinical and laboratory diagnosis was .47, p < .000. 3 AK therapy localizations had a significant correlation with the laboratory diagnosis (p < .05). AK enhanced but did not replace clinical/laboratory diagnosis of thyroid dysfunction. Evidence indicated a significant correlation between certain AK tests and an elevated LDH in the serum. |
To be valid in this new model the MMT would have to reliably sample components of both the central and peripheral nervous systems and be performed in the context of a new, more holistic conceptual model of functional neurology. The future of chiropractic MMT research will depend upon demonstrating the validity and reliability of the MMT for evaluating these types of dysfunctions affecting the anterior horn motor neuron pool.
Understanding normal neuromuscular mechanisms is essential to identifying abnormal and also being able to physically test them. In this way the practitioner may be able to specifically determine areas of dysfunction and thereby individualize the treatment given. More importantly, MMT may allow the neuromuscular system to be used interactively (by examiner and patient) and as a key element in the assessment and treatment of the functional disorders of the patient. This ability to 'manipulate' the neuromuscular system, with an aim of changing the patient's muscular function, postural balance and strength, and to measure the outcome is conceptually an important component of the chiropractic and AK approach to health care. If a patient's injury causes pain and dysfunction, an effective therapy may not only be in the elimination of pain but also an improvement in muscle function as evidenced by the same method of assessment originally used to diagnose the problem. This may add an important measure of objectivity to clinical practice, and potentially increase a patient's awareness about their body and their body's ability for improvement as a result of the therapy given.
To provide the strongest evidence for the use of chiropractic MMT techniques, more randomized controlled clinical trials (RCTs) and systematic reviews will be essential. Although RCTs will be required to document a cause-effect relationship between treatment and outcome, they are frequently impractical projects for the practicing clinician. This is frustrating because it is the clinician who depends on scientific proof that these techniques work.
One alternative is for groups such as ICAK and those who use AK and MMT methods to organize and fund these RCT's. Work so far in this area remains largely limited to reliability and observational studies. Unfortunately, there have not been significant efficacy studies in this area, nor have there been many significant efficacy studies conducted in the chiropractic research arena in general [].
Nineteen examples of peer-reviewed published case reports using MMT and chiropractic AK protocols are presented in Table Table5.5. These 19 case studies demonstrate how the practicing clinician may help narrow the gap between practice and research.
Although case reports cannot prove a treatment's effectiveness, they can describe the performance of techniques in a way that can initiate an hypothesis for a future RCT. More case reports may also add to the body of knowledge in the field of chiropractic AK and MMT.
Conclusion
After 42 years of development and research, the chiropractic profession's use of MMT and AK chiropractic technique has become one of the many diagnostic methods from which some doctors of chiropractic draw their clinical procedures.
In the last forty years we have become more aware of the nervous system. This awareness has allowed us to evaluate patients more completely and from an integrated neuromuscular perspective. This holistic system of approach for the evaluation of neuromuscular function continues to be updated on a regular basis with new and exciting research. Much of the evaluation and treatment of patients using MMT and manual methods remains and will always remain an art. However, we must provide these artistic endeavors with a solid scientific foundation.
Although this narrative literature review offers considerable evidence about the reliability and validity of MMT as an examination tool, most of the rigorous, systematic research on this form of examination has emerged in just the past 30 years. Although evaluation of patients using MMT methods have been investigated with RCTs, prospective (cohort) studies, retrospective studies, single-subject case series and case reports, many questions about the MMT remain unanswered.
One shortcoming is the lack of RCTs to substantiate (or refute) the clinical utility (efficacy, effectiveness) of chiropractic interventions based on MMT findings. Also, because the etiology of a muscle weakness may be multifactorial, any RCT that employs only one mode of therapy to only one area of the body may produce outcomes that are poor due to these limitations.
A limitation of this review may involve research published outside the main databases searched, as well as research articles involving some form of muscle testing but not using the terms manual muscle test, manual muscle testing, or applied kinesiology as they may not have been accessed and included here. In addition this paper has not critically rated each study for its internal and external validity. Such a systematic review should be the subject of future research.
Throughout this paper we have tried to answer the question, 'Are AK and MMT worthy of scientific merit?' In order to evaluate the effectiveness of MMT in the diagnosis of patients with musculoskeletal and nervous system problems, it is necessary to survey the full range of research studies that have addressed the topic, giving due consideration to the strengths and weaknesses of the studies in the literature.
Hopefully this literature review has stimulated a desire for others to review the current MMT literature and become an effective user of and contributor to chiropractic MMT research [125,126].
Competing interests
SCC is a Board Member for the International College of Applied Kinesiology (I.C.A.K.). GJG is the Research Director and Founder of the I.C.A.K. SCC and GJG both employ MMT and AK methods in their evaluation and treatment of patients.
Authors' contributions
SCC and GJG conceived the research idea. SCC acquired the papers and constructed the literature review. SCC and GJG critically appraised the studies. SCC and GJG drafted the manuscript and approved the final version for publication.
References
- Coulter ID. Chiropractic: a philosophy for alternative health care. Oxford: Butterworth-Heinemann; 1999. [Google Scholar]
- Strang V. Essential principles of chiropractic. Davenport, IA: Palmer College of Chiropractic; 1984. [Google Scholar]
- Green BN, Gin RH. George Goodheart, Jr., D.C., and a history of applied kinesiology. J Manipulative Physiol Ther. 1997;20:331–337. [PubMed] [Google Scholar]
- Walther DS. Applied Kinesiology, Synopsis. 2. Pueblo, CO: Systems DC; 2000. [Google Scholar]
- Walther DS. Applied Kinesiology, Chapter 6. In: Coughlin P, editor. Principles and Practice of Manual Therapeutics: Medical Guides to Complementary & Alternative Medicine. Philadelphia: Churchill-Livingstone: Elsevier Science; 2002. [Google Scholar]
- Goodheart GJ. Applied Kinesiology Research Manuals. Detroit, MI: Privately published yearly; 1964. [Google Scholar]
- Frost R. Applied Kinesiology: A training manual and reference book of basic principals and practices. Berkeley, CA: North Atlantic Books, Berkeley; 2002. [Google Scholar]
- Leaf D. Applied Kinesiology Flowchart Manual, III. Plymouth, MA: Privately published; 1995. [Google Scholar]
- Maffetone P. Complementary Sports Medicine: Balancing traditional and nontraditional treatments. Champaign, IL: Human Kinetics; 1999. [Google Scholar]
- Christensen MG, Delle Morgan DR. National Board of Chiropractic Examiners. Greeley, CO; 1993. Job analysis of chiropractic: a project report, survey analysis, and summary of the practice of chiropractic within the United States; p. 78. [Google Scholar]
- Christensen MG, Delle Morgan DR. National Board of Chiropractic Examiners. Vol. 92. Greeley, CO; 1994. Job analysis of chiropractic in Australia and New Zealand: a project report, survey analysis, and summary of the practice of chiropractic within Australia and New Zealand; p. 152. [Google Scholar]
- American Chiropractic Association Database http://www.amerchiro.org/techniques Accessed February 15, 2007.
- LeBoeuf C. A Survey of Registered Chiropractors Practicing in South Australia in 1986. J Aust Chiro Assoc. 1988. pp. 105–10.
- Touch for Health Database http://www.touch4health.com/books.htm Accessed February 15, 2007 See also: A moment of silence for Dr. John Thie, Dynamic Chiropractic 2005;23(19). http://www.chiroweb.com/archives/23/19/11.html.
- Swinkels RA, Bouter LM, Oostendorp RA, Swinkels-Meewisse IJ, Dijkstra PU, de Vet HC. Construct validity of instruments measuring impairments in body structures and function in rheumatic disorders: which constructs are selected for validation? A systematic review. Clin Exp Rheumatol. 2006;24:93–102. [PubMed] [Google Scholar]
- Kaminski M, Boal R, Gillette RG, Peterson DH, Vilinave TJ. A model for the evaluation of chiropractic methods. J Manipulative Physiol Ther. 1987;10:61–4. [PubMed] [Google Scholar]
- Fletcher RH, Fletcher SW, Wagner EH. Clinical epidemiology: the essentials. 3. Philadelphia, PA: Williams & Wilkins; 1988. [Google Scholar]
- Janda V. PhD thesis. Charles University, Prague; 1964. Movement patterns in the pelvic and hip region with special reference to pathogenesis of vertebrogenic disturbances. [Google Scholar]
- Bohannon RW. Manual muscle testing: does it meet the standards of an adequate screening test? Clin Rehabil. 2005;19:662–7. doi: 10.1191/0269215505cr873oa. [PubMed] [CrossRef] [Google Scholar]
- Karin Harms-Ringdahl. Muscle Strength. Edinburgh: Churchill Livingstone; 1993. [Google Scholar]
- Kendall FP, McCreary EK, Provance PG. Muscles: Testing and Function. Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- Daniels L, Worthingham K. Muscle Testing – Techniques of Manual Examination. 7. Philadelphia, PA: W.B. Saunders Co; 2002. [Google Scholar]
- Walther DS. Applied Kinesiology, Synopsis. 2. Pueblo, CO: Systems DC; 2000. [Google Scholar]
- Barbano RL. Handbook of Manual Muscle Testing Neurology. 2000. p. 1211.
- Martin EG, Lovett RW. A method of testing muscular strength in infantile Paralysis. JAMA. pp. 1512–3. 1915 Oct 30.
- Lovett RW, Martin EG. Certain aspects of infantile paralysis with a description of a method of muscle testing. JAMA. pp. 729–33. 1916 Mar 4.
- Shambaugh P. Changes in Electrical Activity in Muscles Resulting from Chiropractic Adjustment: A Pilot Study. J Manipulative Physiol Ther. 1987;10:300–304. [PubMed] [Google Scholar]
- Koes BW, Bouter LM, van Mameren H, et al. A blinded randomized clinical trial of manual therapy and physiotherapy for chronic back and neck complaints: physical outcome measures. J Manipulative Physiol Ther. 1992;15:16–23. [PubMed] [Google Scholar]
- Koes BW, Bouter LM, van Mameren H, et al. Randomized clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow up. BMJ. 1992;304:601.[PMC free article] [PubMed] [Google Scholar]
- Meade TW, Dyer S, Browne W, et al. Low back pain of mechanical origin: randomized comparison of chiropractic and hospital outpatient treatment. BMJ. 1990;300:1431.[PMC free article] [PubMed] [Google Scholar]
- Fleiss JL. The Design and Analysis of Clinical Experiments. New York: John Wiley & Sons; 1986. [Google Scholar]
- Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol. 1990;43:543–9. doi: 10.1016/0895-4356(90)90158-L. [PubMed] [CrossRef] [Google Scholar]
- Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ. 304:1491–4. 1992 Jun 6. [PMC free article] [PubMed] [Google Scholar]
- Florence JM, Pandya S, King WM, Robison JD, Signore LC, Wentzell M, Province MA. Clinical trials in Duchenne dystrophy. Standardization and reliability of evaluation procedures. Phys Ther. 1984;64:41–5. [PubMed] [Google Scholar]
- Mendell JR, Florence J. Manual muscle testing. Muscle Nerve. 1990;13:S16–20. doi: 10.1002/mus.880131307. [PubMed] [CrossRef] [Google Scholar]
- Caruso B, Leisman G. A Force/Displacement Analysis of Muscle Testing. Perceptual and Motor Skills. 2000;91:683–692. [PubMed] [Google Scholar]
- Lilienfeld AM, Jacobs M, Willis M. A study of the reproducibility of muscle testing and certain other aspects of muscle scoring. Phys Ther Rev. 1954;34:279–289. [PubMed] [Google Scholar]
- Blair L. The role of the physical therapist in the evaluation studies of the poliomyelitis vaccine field trials. Phys Ther Rev. 1955;37:437–447. [PubMed] [Google Scholar]
- Iddings DM, Smith LK, Spencer WA. Muscle testing: part 2. Reliability in clinical use. Phys Ther Rev. 1961;41:249–256. [PubMed] [Google Scholar]
- Silver M, McElroy A, Morrow L, Heafner BK. Further standardization of manual muscle test for clinical study: applied in chronic renal disease. Phys Ther. 1970;50:1456–1466. [PubMed] [Google Scholar]
- Frese E, Brown M, Norton BJ. Clinical Reliability of Manual Muscle Testing. Phys Ther. 1987;67:1072–1076. [PubMed] [Google Scholar]
- Barr AE, Diamond BE, Wade CK, Harashima T, Pecorella WA, Potts CC, Rosenthal H, Fleiss JL, McMahon DJ. Reliability of testing measures in Duchenne or Becker muscular dystrophy. Arch Phys Med Rehabil. 1991;72:315–319. [PubMed] [Google Scholar]
- Perry J, Weiss WB, Burnfield JM, Gronley JK. The supine hip extensor manual muscle test: a reliability and validity study. Arch Phys Med Rehabil. 2004;85:1345–50. doi: 10.1016/j.apmr.2003.09.019. [PubMed] [CrossRef] [Google Scholar]
- Jacobs G. Applied kinesiology: an experimental evaluation by double blind methodology. J Manipulative Physiol Ther. 1981;4:141–145.[Google Scholar]
- Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther. 1987;67:1342–1347. [PubMed] [Google Scholar]
- Hsieh CY, Phillips RB. Reliability of Manual Muscle Testing with a Computerized Dynamometer. J Manipulative Physiol Ther. 1990;13:72–82. [PubMed] [Google Scholar]
- Florence JM, Pandya S, King WM, Robison JD, Baty J, Miller JP, Schierbecker J, Signore LC. Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne's muscular dystrophy. Phys Ther. 1992;72:115–22. discussion 122-6. [PubMed] [Google Scholar]
- Lawson A, Calderon L. Interexaminer Agreement for Applied Kinesiology Manual Muscle Testing. Percepl Mot Skills. 1997;84:539–546. [PubMed] [Google Scholar]
- Leisman G, Zenhausern R, Ferentz A, Tefera T, Zemcov A. Electromyographic effects of fatigue and task repetition on the validity of estimates of strong and weak muscles in applied kinesiological muscle-testing procedures. Percept Mot Skills. 1995;80:963–77. [PubMed] [Google Scholar]
- Marino M, Nicholas JA, Gleim GW, Rosenthal P, Nicholas SJ. The efficacy of manual assessment of muscle strength using a new device. Am J Sports Med. 1982;10:360–4. [PubMed] [Google Scholar]
- Basmajian JV. Muscles Alive – Their Functions Revealed by Electromyography. 4. Baltimore, MD: Williams & Wilkins Co; 1978. [Google Scholar]
- MacConaill NA, Basmajian JV. Muscles and Movements – A Basis for Human Kinesiology. Huntington, NY: Robert E. Krieger Publishing Co; 1977. [Google Scholar]
- Rosenbaum R. Carpal tunnel syndrome and the myth of El Dorado. Muscle & Nerve. 1999;22:1165–1167. doi: 10.1002/(SICI)1097-4598(199909)22:9<1165::AID-MUS1>3.0.CO;2-1. [PubMed] [CrossRef] [3.0.CO;2-1&' target='pmc_ext' ref='reftype=other&article-id=1847521&issue-id=141525&journal-id=321&FROM=Article%7CCitationRef&TO=Content%20Provider%7CLink%7CGoogle%20Scholar'>Google Scholar]
- Pollard HP, Bablis P, Bonello R. Can the Ileocecal Valve Point Predict Low Back Pain Using Manual Muscle Testing? Chiropr Aust. 2006;36:58–62.[Google Scholar]
- Pollard H, Lakay B, Tucker F, Watson B, Bablis P. Interexaminer reliability of the deltoid and psoas muscle test. J Manipulative Physiol Ther. 2005;28:52–6. doi: 10.1016/j.jmpt.2004.12.008. [PubMed] [CrossRef] [Google Scholar]
- Escolar DM, Henricson EK, Mayhew J, Florence J, Leshner R, Patel KM, Clemens PR. Clinical evaluator reliability for quantitative and manual muscle testing measures of strength in children. Muscle Nerve. 2001;24:787–93. doi: 10.1002/mus.1070. [PubMed] [CrossRef] [Google Scholar]
- Perot C, Meldener R, Gouble F. Objective Measurement of Proprioceptive Technique Consequences on Muscular Maximal Voluntary Contraction During Manual Muscle Testing. Agressologie. 1991;32:471–474. [PubMed] [Google Scholar]
- Payton OD. Research: The Validation of Clinical Experience. Philadelphia, FA Davis; 1994. [Google Scholar]
- Kendall HO, Kendall FP, Boynton DA. Posture and Pain. Baltimore: Williams & Wilkins Company; 1952. [Google Scholar]
- Janda V. Muscle Function Testing. London: Butterworths; 1983. [Google Scholar]
- A number of chiropractic 'name techniques' have evolved from AK that also employ MMT as part of their diagnostic system, including: Neuro Emotional Technique (N.E.T.); Neural Organization Technique (N.O.T.); Clinical Kinesiology; Contact Reflex Analysis (C.R.A.); Total Body Modification (T.B.M.), and others
- Schmitt WH, Yannuck SF. Expanding the Neurological Examination Using Functional Neurological Assessment Part II: Neurologic Basis of Applied Kinesiology. Intern J Neuroscience. 1999;97:77–108. [PubMed] [Google Scholar]
- Lamb RI. Manual Muscle Testing. In: Rothstein JM, editor. Measurement in physical therapy. New York: Churchill Livingstone; 1985. pp. 47–55. [Google Scholar]
- Michener LA, Boardman ND, Pidcoe PE, Frith AM. Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther. 2005;85:1128–38. [PubMed] [Google Scholar]
- Great Lakes ALS Study Group A comparison of muscle strength testing techniques in amyotrophic lateral sclerosis. Neurology. 61:1503–7. 2003 Dec 9. [PubMed] [Google Scholar]
- Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, DePrince M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001;80:572–7. doi: 10.1097/00002060-200108000-00005. [PubMed] [CrossRef] [Google Scholar]
- Panjabi M. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J. 2005 Jul 27. [PMC free article] [PubMed]
- Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13:361–70. doi: 10.1016/S1050-6411(03)00042-7. [PubMed] [CrossRef] [Google Scholar]
- Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2:357–71. doi: 10.1016/S1529-9430(02)00400-X. [PubMed] [CrossRef] [Google Scholar]
- Lund JP, Donga R, Widmer CG, Stohler CS. The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Canadian Journal of Physiology and Pharmacology. 1991;69:683–694. [PubMed] [Google Scholar]
- Falla DL, Jull GA, Hodges PW. Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine. 29:2108–14. 2004 Oct 1. [PubMed] [Google Scholar]
- Mellor R, Hodges PW. Motor unit synchronization is reduced in anterior knee pain. J Pain. 2005;6:550–8. doi: 10.1016/j.jpain.2005.03.006. [PubMed] [CrossRef] [Google Scholar]
- Cowan SM, Schache AG, Brukner P, Bennell KL, Hodges PW, Coburn P, Crossley KM. Delayed onset of transversus abdominus in long-standing groin pain. Med Sci Sports Exerc. 2004;36:2040–5. doi: 10.1249/01.MSS.0000147587.81762.44. [PubMed] [CrossRef] [Google Scholar]
- Cowan SM, Bennell KL, Hodges PW, Crossley KM, McConnell J. Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2001;82:183–9. doi: 10.1053/apmr.2001.19022. [PubMed] [CrossRef] [Google Scholar]
- Nummi J, Jarvinen T, Stambej U, Wickstrom G. Diminished dynamic performance capacity of back and abdominal muscles in concrete reinforcement workers. Scand J Work Environ Health. 1978;4:39–46. [PubMed] [Google Scholar]
- Addison R, Schultz A. Trunk strengths in patients seeking hospitalization for chronic low-back disorders. Spine. 1980;5:539–44. doi: 10.1097/00007632-198011000-00009. [PubMed] [CrossRef] [Google Scholar]
- Karvonen MJ, Viitasalo JT, Komi PV, Nummi J, Jarvinen T. Back and leg complaints in relation to muscle strength in young men. Scand J Rehabil Med. 1980;12:53–9. [PubMed] [Google Scholar]
- MacNeill T, Warwick D, Andersson G, Schultz A. Trunk strength in attempted flexion, extension, and lateral bending in healthy subjects and patients with low-back disorders. Spine. 1980;5:529–38. [PubMed] [Google Scholar]
- Nordgren B, Schele R, Linroth K. Evaluation and prediction of back pain during military field service. Scand J Rehabil Med. 1980;12:1–8. [PubMed] [Google Scholar]
- Mayer TG, Gatchel RJ, Kischino N, Keeley J, Capra P, Mayer H, Barnett J, Mooney V. Objective assessment of spine function following industrial injury. A prospective study with comparison group and one-year follow-up. Spine. 1985;10:482–93. doi: 10.1097/00007632-198507000-00002. [PubMed] [CrossRef] [Google Scholar]
- Rantanen J, Hurme M, Falck B, Alaranta H, Nykvist F, Lehto M, Einola S, Kalimo H. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine. 1993;18:568–74. doi: 10.1097/00007632-199304000-00008. [PubMed] [CrossRef] [Google Scholar]
- Hides JA, Richardson CA, Jull G. Multifidus muscle recovery is not automatic after resolution of acute first-episode low back pain. Spine. 1996;21:2763–2769. doi: 10.1097/00007632-199612010-00011. [PubMed] [CrossRef] [Google Scholar]
- Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. Spine. 1996;21:2640–2650. doi: 10.1097/00007632-199611150-00014. [PubMed] [CrossRef] [Google Scholar]
- Chaffin DB, Park KS. A longitudinal study of low-back pain as associated with occupational weight lifting factors. Am Ind Hyg Assoc J. 1973;34:513–25. [PubMed] [Google Scholar]
- Biering-Sorensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9:106–19. doi: 10.1097/00007632-198403000-00002. [PubMed] [CrossRef] [Google Scholar]
- Mayer TG, Barnes D, Nichols G, Kishino ND, Coval K, Piel B, Hoshino D, Gatchel RJ. Progressive isoinertial lifting evaluation. II. A comparison with isokinetic lifting in a disabled chronic low-back pain industrial population. Spine. 1988;13:998–1002. doi: 10.1097/00007632-198809000-00006. [PubMed] [CrossRef] [Google Scholar]
- Nachemson A, Lindh M. Measurement of abdominal and back muscle strength with and without low back pain. Scand J Rehabil Med. 1969;1:60–3. [PubMed] [Google Scholar]
- Cox JM. Low Back Pain: Mechanism, Diagnosis and Treatment. Sixth. Baltimore: William & Wilkins; 1999. p. 439, 406. [Google Scholar]
- Goodall RM, Hammes MR. Electronic comparison of toe strengths for diagnosis of lumbar nerve root lesions. Med Biol Eng Comput. 1986;24:555–557. doi: 10.1007/BF02443976. [PubMed] [CrossRef] [Google Scholar]
- Hossain M, Nokes LDM. A model of dynamic sacro-iliac joint instability from malrecruitment of gluteus maximus and biceps femoris muscles resulting in low back pain. Medical Hypotheses. 2005;65:278–281. doi: 10.1016/j.mehy.2005.02.035. [PubMed] [CrossRef] [Google Scholar]
- Triano J, Schultz A. Correlation of objective measure of trunk motion and muscle function with low-back disability ratings. Spine. 1987;12:561–5. doi: 10.1097/00007632-198707000-00010. [PubMed] [CrossRef] [Google Scholar]
- McNeill T, Warwick D, Andersson G, Schultz A. Trunk strengths in attempted flexion, extension, and lateral bending in healthy subjects and patients with low-back disorders. Spine. 1980;5:529–38. doi: 10.1097/00007632-198011000-00008. [PubMed] [CrossRef] [Google Scholar]
- Jepsen JR, Laursen LH, Hagert CG, Kreiner S, Larsen AI. Diagnostic accuracy of the neurological upper limb examination I: inter-rater reproducibility of selected findings and patterns. BMC Neurol. 6:8. doi: 10.1186/1471-2377-6-8. 2006 Feb 16. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Deyo R. Understanding the accuracy of diagnostic tests. In: Weinstein JN, Rydevik ABL, Sonntag VKH, editor. Essentials of the Spine. New York: Raven Press; 1995. p. 65. [Google Scholar]
- Bohannon RW. Measuring knee extensor muscle strength. Am J Phys Med Rehabil. 2001;80:13–8. doi: 10.1097/00002060-200101000-00004. [PubMed] [CrossRef] [Google Scholar]
- Schwartz S, Cohen ME, Herbison GJ, Shah A. Relationship between two measures of upper extremity strength: manual muscle test compared to hand-held myometry. Arch Phys Med Rehabil. 1992;73:1063–8. [PubMed] [Google Scholar]
- Bohannon RW. Manual muscle test scores and dynamometer test scores of knee extension strength. Arch Phys Med Rehabil. 1986;67:390–2. [PubMed] [Google Scholar]
- Triano J, Davis B. Experimental Characterization of The Reactive Muscle Phenomenon. Chiro Econ. 1976. pp. 44–50.
- Niemuth PE, Johnson RJ, Myers MJ, Thieman TJ. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005;15:14–21. doi: 10.1097/00042752-200501000-00004. [PubMed] [CrossRef] [Google Scholar]
- Moncayo R, Moncayo H, Ulmer H, Kainz H. New diagnostic and therapeutic approach to thyroid-associated orbitopathy based on applied kinesiology and homeopathic therapy. J Altern Complement Med. 2004;10:643–50. [PubMed] [Google Scholar]
- Rainville J, Jouve C, Finno M, Limke J. Comparison of four tests of quadriceps strength in L3 or L4 radiculopathies. Spine. 28:2466–71. doi: 10.1097/01.BRS.0000090832.38227.98. 2003 Nov 1. [PubMed] [CrossRef] [Google Scholar]
- Hungerford B, Gilleard W, Hodges P. Evidence of Altered Lumbopelvic Muscle Recruitment in the Presence of Sacroiliac Joint Pain. Spine. 2003;28:1593–1600. doi: 10.1097/00007632-200307150-00022. [PubMed] [CrossRef] [Google Scholar]
- Monti D, Sinnott J, Marchese M, Kunkel E, Greeson J. Muscle Test Comparisons of Congruent and Incongruent Self-Referential Statements. Perceptual and Motor Skills. 1999;88:1019–1028. [PubMed] [Google Scholar]
- Schmitt W, Leisman G. Correlation of Applied Kinesiology Muscle Testing Findings with Serum Immunoglobulin Levels for Food Allergies. International Journal of Neuroscience. 1998;96:237–244. [PubMed] [Google Scholar]
- Goodheart G. Proc Inter Conf Spinal Manip. Washington, DC; 1990. Failure of the musculo-skeletal system may produce major weight shifts in forward and backward bending; pp. 399–402. [Google Scholar]
- Scopp A. An Experimental Evaluation of Kinesiology in Allergy and Deficiency Disease Diagnosis. Journal of Orthomolecular Psychiatry. 1979;7:137–8.[Google Scholar]
- Carpenter SA, Hoffmann J, Mendel R. Evaluation of Muscle-Organ Association, Part I and II. J Clin Chiro. 1977;II:22–33. and III(1):42–60. [Google Scholar]
- Haas M, Bronfort G, Evans RL. Chiropractic clinical research: progress and recommendations. J Manipulative Physiol Ther. 2006;29:695–706. doi: 10.1016/j.jmpt.2006.09.005. [PubMed] [CrossRef] [Google Scholar]
- Cuthbert S. Proposed mechanisms and treatment strategies for motion sickness disorder: A case series. J Chiro Med Spring. 2006;5:22–31.[PMC free article] [PubMed] [Google Scholar]
- Cuthbert S, Blum C. Symptomatic Arnold-Chiari malformation and cranial nerve dysfunction: a case study of applied kinesiology cranial evaluation and treatment. J Manipulative Physiol Ther. 2005;28:e1–6. doi: 10.1016/j.jmpt.2005.03.001. [PubMed] [CrossRef] [Google Scholar]
- Meldener R. Post-surgical hip dislocation. Int J AK and Kinesio Med. 2005;19:27.[Google Scholar]
- Chung AL, Shin EJ, Yoo IJ, Kim KS. Reliability of the kinesiologic occlusal position. Int J AK and Kinesio Med. 2005;20:6–10.[Google Scholar]
- Caso ML. Evaluation of Chapman's neurolymphatic reflexes via applied kinesiology: a case report of low back pain and congenital intestinal abnormality. J Manipulative Physiol Ther. 2004;27:66. doi: 10.1016/j.jmpt.2003.11.009. [PubMed] [CrossRef] [Google Scholar]
- Cuthbert S. Applied Kinesiology and Down syndrome: a study of 15 cases. Int J AK and Kinesio Med. 2003;16:16–21.[Google Scholar]
- Maykel W. Pediatric case history: cost effective treatment of block naso-lacrimal canal utilizing applied kinesiology tenets. Int J AK and Kinesio Med. 2003;16:34.[Google Scholar]
- Weiss G. A 39-year-old female cyclist suffering from total exhaustion caused by over-training and false nutrition. Int J AK and Kinesio Med. 2003;15:39.[Google Scholar]
- Sprieser PT. Episodic paroxysmal vertigo. Int J AK and Kinesio Med. 2002;14:35.[Google Scholar]
- Leaf D. Severe equilibrium problems non-responsive to pharmacological care treated with chiropractic and applied kinesiology: a case history. Int J AK and Kinesio Med. 2002;13:27.[Google Scholar]
- Gregory WM, Mills SP, Hamed HH, Fentiman IS. Applied kinesiology for treatment of women with mastalgia. Breast. 2001;10:15–9. doi: 10.1054/brst.2000.0176. [PubMed] [CrossRef] [Google Scholar]
- Cuthbert S. An applied kinesiology evaluation of facial neuralgia: a case history of Bell's Palsy. Int J AK and Kinesio Med. 2001;10:42–45.[Google Scholar]
- Calhoon J. Applied Kinesiology management of multiple sclerosis: a case history. Int J AK and Kinesio Med. 2001;12:28–29.[Google Scholar]
- Mathews MO, Thomas E, Court L. Applied Kinesiology Helping Children with Learning Disabilities. Int J AK and Kinesio Med. 1999. p. 4.
- Masarsky CS, Weber M. Somatic dyspnea and the orthopedics of respiration. Chiro Tech. 1991;3:26–29.[Google Scholar]
- Masarsky CS, Weber M. Chiropractic Management of Chronic Obstructive Pulmonary Disease. J Manipulative Physiol Ther. 1988;11:505–510. [PubMed] [Google Scholar]
- ICAK-International and ICAK USA websites, 'Applied Kinesiology Research and Literature Compendium' http://www.icak.com/college/research/publishedarticles.shtml and http://www.icakusa.com/ Accessed February 15, 2007.
- Sacro Occipital Technique Organization website http://www.sotousa.org/SOTLiterature/Applied%20Kinesiology/Applied%20Kinesiology%20Literature.htm Accessed February 15, 2007.
Abstract
Survivors of acute respiratory distress syndrome (ARDS) and other causes of critical illness often have generalized weakness, reduced exercise tolerance, and persistent nerve and muscle impairments after hospital discharge.1-6 Using an explicit protocol with a structured approach to training and quality assurance of research staff, manual muscle testing (MMT) is a highly reliable method for assessing strength, using a standardized clinical examination, for patients following ARDS, and can be completed with mechanically ventilated patients who can tolerate sitting upright in bed and are able to follow two-step commands. 7, 8
This video demonstrates a protocol for MMT, which has been taught to ≥43 research staff who have performed >800 assessments on >280 ARDS survivors. Modifications for the bedridden patient are included. Each muscle is tested with specific techniques for positioning, stabilization, resistance, and palpation for each score of the 6-point ordinal Medical Research Council scale.7,9-11 Three upper and three lower extremity muscles are graded in this protocol: shoulder abduction, elbow flexion, wrist extension, hip flexion, knee extension, and ankle dorsiflexion. These muscles were chosen based on the standard approach for evaluating patients for ICU-acquired weakness used in prior publications. 1,2.
Protocol
1. Introduction
During manual muscle testing (MMT), each muscle group is tested bilaterally. For demonstration purposes, only one side is tested in this video for each of the 6 muscle groups. One hand of the examiner applies resistance or palpates the muscle or tendon for contraction while the other hand stabilizes the extremity being tested to keep it in the test position. The test is repeated if the patient does not understand the instructions or is not applying maximum effort.
2. Grading follows the Medical Research Council (MRC) system (Table 1).1
Figure 1 illustrates an algorithm for the MRC muscle strength scoring system. If the subject is missing a limb, has a cast, or is unable to be placed in the correct testing position, muscle strength is graded as 'unable to assess'. If the patient has a fixed contracture, but can otherwise perform the test, the muscle is graded. Medical devices, such as catheters and drains, and mechanical ventilation usually do not impede muscle testing, unless a joint is immobilized to ensure proper functioning of a device.
Figure 1. Manual Muscle Testing Algorithm
3. Procedure
For each muscle tested, the examiner stands to the side being tested, and the patient is sitting upright and positioned to allow full movement of the joint against gravity. The examiner demonstrates the desired movement against gravity. The examiner then requests the patient to repeat the motion.
If the patient can move through the desired range of motion against gravity, the examiner attempts to apply resistance in the testing position while stating 'Hold it, don't let me push it down' or 'Hold it, don't let me bend it' (Figure 2). If the patient tolerates no resistance, the muscle score is Grade 3. If the patient tolerates some resistance, the score is Grade 4, and full resistance, Grade 5.
If the patient cannot move against gravity, the patient is repositioned to allow movement of the extremity with gravity eliminated. If supporting the limb, the examiner provides neither assistance nor resistance to the patient's voluntary movement. This gravity-eliminated positioning will vary for each muscle tested. If the patient cannot complete at least partial range of motion with gravity eliminated, the muscle or tendon is observed and/or palpated for contraction.
For a bedridden patient who cannot sit up in a bed placed in the chair position or on the edge of the bed, alternate positions for testing the lower extremity are included in this protocol.
4. Shoulder Abduction
Testing position - arm out from the side at shoulder level. The examiner demonstrates the motion, then states 'Lift your arm out to the side to shoulder level.' The hand giving resistance is contoured over the patient's arm just above the elbow. The other hand stabilizes the shoulder above the shoulder joint. The examiner states 'Hold it, don't let me push it down.' To assess grades 3, 4, or 5, please see section 3.2 above.
If weaker than Grade 3, the patient lies supine with arms at the side. The examiner supports the arm just above the elbow and at the wrist to assure that the shoulder does not externally rotate (turn outward). The patient attempts to move the arm out to the side. The examiner states: 'Try to move your arm out to the side'. Grade 2 is assigned if the patient moves with gravity eliminated.
If weaker than Grade 2, the examiner states ' Try to move your arm out to the side ' and palpates the middle deltoid muscle, as demonstrated, for contraction, and scores as Grade 1 or 0 as previously defined.
Shoulder MMT can be performed with central venous catheters (e.g., subclavian and jugular) in place, including those used for dialysis. (Figure 2)
The remaining assessments will be completed similarly to above using specific test positions for the patient and examiner, and specific instructions for the patient's movement.
5. Elbow Flexion
Test position - forearm supinated and flexed slightly more than 90 degrees. Verbal instructions: 'Bend your elbow slightly more than 90 degrees'. The hand giving resistance is contoured over the flexor surface of the forearm proximal to the wrist. The examiner's other hand applies counterforce by cupping the palm over the anterior superior aspect of the shoulder. The examiner then states: 'Hold it. Don't let me push it down' and scores Grades 3, 4, or 5 as previously described.
If weaker than Grade 3, the shoulder is abducted to 90 degrees. The examiner supports the arm under the elbow and, if necessary, the wrist as well. The forearm is turned with the thumb facing the ceiling. With the elbow extended, the patient attempts to flex the elbow. The examiner states: 'Try to bend your elbow.' Grade 2 is assigned if the patient can flex the elbow.
If weaker than Grade 2, the forearm is supinated and positioned at the side in approximately 45 degrees of elbow flexion. The examiner states 'Try to bend your elbow', palpates the biceps tendon and scores as either Grade 1 or 0.
6. Wrist Extension
Test position - arm at the side, elbow flexed to 90 degrees with the forearm pronated and the wrist fully extended. Verbal instructions: 'Bend your wrist up as far as possible.' The examiner's hand giving resistance is placed over the back of the patient's hand just distal to the wrist. The examiner's other hand supports the patient's forearm. The examiner then states: 'Hold it. Don't let me push it down' and scores Grades 3, 4 or 5.
If weaker than Grade 3, the elbow is flexed to 90 degrees and forearm turned with thumb facing the ceiling. The forearm and wrist are supported by the examiner. The examiner states: 'Bend your hand toward me'. Grade 2 is assigned if the patient can extend the wrist.
If weaker than Grade 2, the examiner states 'Bend your wrist toward me' and palpates the two extensor tendons, one on each side of the wrist, as demonstrated, and scores as Grade 1 or 0. The examiner is careful not to palpate the tendons in the middle of the wrist.
This test is not performed if there is an ipsilateral radial arterial catheter in place.
7. Hip Flexion
Test position - sitting with the hip fully flexed and knee bent. The patient may place their hands on the bed or table for stability. Verbal instructions: 'Raise your knee up as high as it will go.' The examiner's hand giving resistance is placed on top of the thigh just proximal to the knee. The other hand provides stability at the side of the hip. The examiner then states: 'Hold it. Don't let me push it down' and scores Grades 3, 4 or 5.
If weaker than Grade 3, the patient lays down on the side not being tested. For example, the patient lays on the right side to test the left hip. The examiner stands behind the patient with one arm cradling the leg being tested with the hand supporting under the knee. The opposite hand maintains alignment of the trunk at the hip. The examiner states:'Bring your knee toward your chest.' Grade 2 is assigned if the patient can flex the hip.
If weaker than Grade 2, the patient is supine. The examiner asks, 'May I touch your leg here?' (pointing to the inner aspect of the hip joint). With the patient's permission, the examiner states 'Bend your hip' and palpates the iliopsoas tendon, as demonstrated, and scores as Grade 1 or 0.
In a bedridden patient, grades 5, 4, and 3 are tested with the bed in the chair position, or the head of the bed elevated as far as possible. Pillows are placed under the knee to flex the hip to 90 degrees. The examiner assures that the foot is lifted off the bed when asking the patient to raise the knee off the bed. Grades 2 and 1 are scored as previously described.
This test can be performed in patients with intact and well secured femoral intravascular catheters. Liquor license value in nj.
8. Knee Extension
Test position - sitting upright with the knee fully extended to 0 degrees. Avoid knee hyperextension. Verbal instructions; 'Straighten your knee'. The hand giving resistance is contoured on top of the leg just proximal to the ankle. The other hand is placed under the thigh above the knee. The examiner then states 'Hold it. Don't let me bend it' and scores Grades 3, 4 or 5.
If weaker than Grade 3, the patient lays on the non-testing side. The examiner stands behind the patient at knee level. The leg not being tested may be flexed for stability. One arm cradles the leg being tested around the thigh with the hand supporting the underside of the knee. The other hand holds the leg just above the ankle. The examiner states: 'Straighten your knee.' Grade 2 is assigned if the patient can extend the knee (Figure 3).
If weaker than Grade 2, the patient is supine and the examiner states:'Push the back of your knee down' or 'Tighten your knee cap' and palpates the quadriceps tendon, and scores as Grade 1 or 0.
For the bedridden patient, in scoring Grades 3, 4,and 5, the patient is positioned in the same manner as for hip flexion and graded as described above for knee extension (Figure 4).
9. Ankle Dorsiflexion
Test position - sitting, with the heel on floor, foot in full dorsiflexion, and shoes and socks removed. Verbal instructions: 'Bend your foot up as far as possible.' The toes are relaxed during the test. The hand giving resistance is cupped over the top of the foot proximal to the toes. The other hand is contoured around the front of the leg just proximal to the ankle. The examiner then states 'Hold it, don't let me push it down' and scores Grade 3, 4 or 5.
If weaker than Grade 3, but there is partial range of motion against gravity, assign Grade 2.
If weaker than Grade 2, palpate the tibialis anterior tendon, and score as Grade 1or 0.
The bedridden patient is tested supine, with the leg extended and a pillow placed under the knee.
This test can usually be applied with an intact and secured pedal intravascular catheter. Be careful not to dislodge the catheter.
10. Representative Results:
MMT using this protocol has excellent inter-rater reliability when applied with both ARDS survivors and simulated patents. Quality assurance of 19 trainees examining 12 muscle groups demonstrated an intraclass correlation coefficient (95% confidence interval [CI]) of 0.99 (0.97-1.00).8 Agreement (kappa; 95% CI) for detecting clinically significant weakness (i.e., composite MRC score <80% of maximum) was 1.00 (0.55-1.00). Previous studies have shown high inter-rater reliability with stroke, amyotrophic lateral sclerosis (ALS), Guillain-Barre, and other critically ill patients.12-14
Figure 2. ICU patient with a left shoulder abduction contracture. MMT with a left radial arterial line, cardiac monitoring, and continuous dialysis through a right internal jugular catheter. The patient is positioned for shoulder abduction MMT Grades 3, 4 and 5.
Figure 3. ICU bedridden patient with a right internal jugular catheter for continuous dialysis. The patient is positioned on the right side for knee extension MMT Grade 2.
Figure 4. ICU bedridden patient with a left knee flexion contracture. The patient is positioned supine with a pillow under the knee for knee extension MMT Grades 3, 4 and 5.
| Table 1. Manual Muscle Test 3 | |
| Grade | Manual Muscle Test |
| 5 | Movement against gravity plus full resistance |
| 4 | Movement against gravity plus some resistance |
| 3 | Completes the available test range of motion against gravity, but tolerates no resistance |
| 2 | The patient completes full or partial range of motion with gravity eliminated |
| 1 | Slight contractility without any movement |
| 0 | No evidence of contractility (complete paralysis) |

Discussion
Depending on the diagnostic criteria, 9 – 87% of ICU patients develop neuromuscular complications, which are associated with prolonged mechanical ventilation, increased hospital stay and rehabilitation time, and potentially associated with increased mortality.1,2,16-18 Periodic reassessment of muscle strength, using a reliable method which minimizes inter-rater variability is helpful to detect changes over time. An important limitation of MMT using the MRC score system is the 6-point ordinal scale. Muscle strength testing using a hand held dynamometer is less commonly used but has the advantage of using a ratio scale for measurement.19 In addition, some ICU patients may not be awake enough to tolerate a MMT exam.2 However, in our experience, once a patient is awake and cooperative, there are only a small number of patients who do not tolerate the exam. If this intolerance is due to poor endurance, the exam can be completed in smaller portions, rather than all at once. The muscle strength grading described in this video has been administered to ICU survivors and to cooperative, critically ill patients even while undergoing mechanical ventilation with intravascular devices in place that do not interfere with joint motion . Recent developments in ICU clinical practice whereby deep sedation is avoided, enhances the ability of mechanically ventilated patients to participate in MMT examination, rehabilitation therapies, and even ambulate while mechanically ventilated.20 Manual muscle testing of the 6 muscle groups described in this video is a simple, reliable, inexpensive method of obtaining a quantitative muscle strength evaluation for patients during and after critical illness.
Acknowledgments
Supported by NIH grant # R01HL088045. Drs. Eddy Fan and Michelle Kho are each supported by a Fellowship Award from the Canadian Institutes of Health Research.
References
- De Jonghe B. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288:2859–2867. [PubMed] [Google Scholar]
- Ali NA. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008;178:261–268. [PubMed] [Google Scholar]
- Angel MJ, Bril V, Shannon P, Herridge MS. Neuromuscular function in survivors of the acute respiratory distress syndrome. Can. J. Neurol. Sci. 2007;34:427–432. [PubMed] [Google Scholar]
- Cheung AM. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2006;174:538–544. [PubMed] [Google Scholar]
- Stevens RD. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–1891. [PubMed] [Google Scholar]
- Herridge MS. One-year outcomes in survivors of the acute respiratory distress syndrome. N. Engl. J. Med. 2003;348:683–693. [PubMed] [Google Scholar]
- Medical Research Council. Aids to the Investigation of the Peripheral Nervous System. London: Her Majesty's Stationary Office; 1976. [Google Scholar]
- Fan E. Inter-rater reliability of manual muscle strength testing in ICU survivors and simulated patients. Intensive Care Med. 2010;34:1038–1043.[PMC free article] [PubMed] [Google Scholar]
- Hislop HJ, Montgomery JM. Daniels and Worthingham's Muscle Testing. St. Louis, Missouri: Saunders Elsevier; 2007. [Google Scholar]
- Reese NB. Muscle and Sensory Testing. St. Louis, Missouri: Saunders Elsevier; 2005. [Google Scholar]
- Kendall FP. Muscles; Testing and Function with Posture and Pain. Baltimore, Maryland: Lippincott Williams and Wilkins; 2005. [Google Scholar]
- Lieu BK, Hough CL. Assessment of Weakness in Critically Ill Patients Using Physical Examination. Am J Respir Crit Care Med. 2007;175:A218–A218.[Google Scholar]
- Gregson JM. Reliability of measurements of muscle tone and muscle power in stroke patients. Age Ageing. 2000;29:223–228. [PubMed] [Google Scholar]
- Great Lakes ALS Study Group . A comparison of muscle strength testing techniques in amyotrophic lateral sclerosis. Neurology. 2003;61:1503–1507. [PubMed] [Google Scholar]
- Kleyweg RP, van der Meche FG, Schmitz PI. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barre syndrome. Muscle Nerve. 1991;14:1103–1109. [PubMed] [Google Scholar]
- Zink W, Kollmar R, Schwab S. Critical illness polyneuropathy and myopathy in the intensive care unit. Nat. Rev. Neurol. 2009;5:372–379. [PubMed] [Google Scholar]
- Sharshar T. Presence and severity of intensive care unit-acquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit. Care Med. 2009;37:3047–3053. [PubMed] [Google Scholar]
- Griffiths RD, Hall JB. Intensive care unit-acquired weakness. Crit. Care Med. 2010;38:779–787. [PubMed] [Google Scholar]
- Bohannon RW. Measuring knee extensor muscle strength. Am J Phys Med Rehabil. 2001;80:13–18. [PubMed] [Google Scholar]
- Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300:1685–1690. [PubMed] [Google Scholar]